157. Overcoming Loneliness & Isolation as a Teen feat. Dr. Caroline Fenkel
listen to this episode:
Tune in and subscribe on your favorite platform: Apple Podcasts | Spotify | Stitcher | Google Play | Radio Public | PocketCasts | Overcast | Breaker | Anchor
Today's guest is Dr. Caroline Fenkel— a leader in adolescent mental healthcare with over fifteen years of direct clinical experience working with youth and families. Dr. Fenkel oversees all aspects of clinical programming at Charlie Health— the largest provider of virtual IOP treatment programs for teens, young adults, and families navigating mental health challenges. We discuss why it’s so important to seek evidence-based treatments for mental health challenges and first steps to take to find treatment, how Covid has affected teen mental health and its treatment, why family systems can often cause loneliness and isolation, negative effects and warning signs of loneliness and isolation, why many teens don’t take the steps to decrease their loneliness and how to break this cycle, ways a teen’s support system can help them to feel less lonely, advice for parents of teens experiencing loneliness, and how teens can increase connectedness and independence.
Dr. Fenkel's Instagram: https://www.instagram.com/dr.c.lcsw/
Mentioned In The Episode…
SHOP GUEST RECOMMENDATIONS: https://amzn.to/3A69GOC
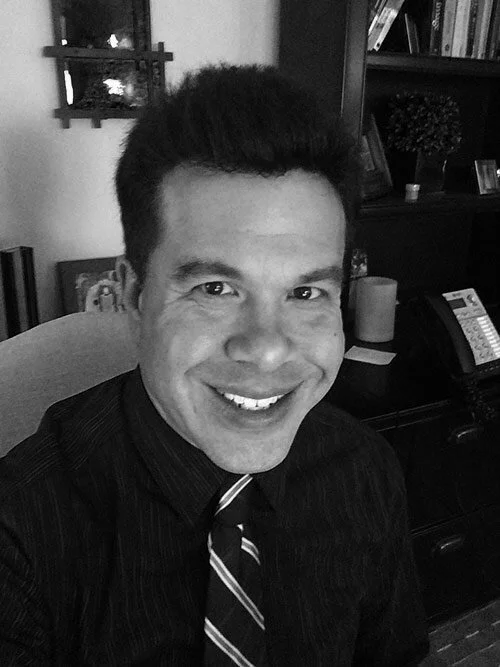
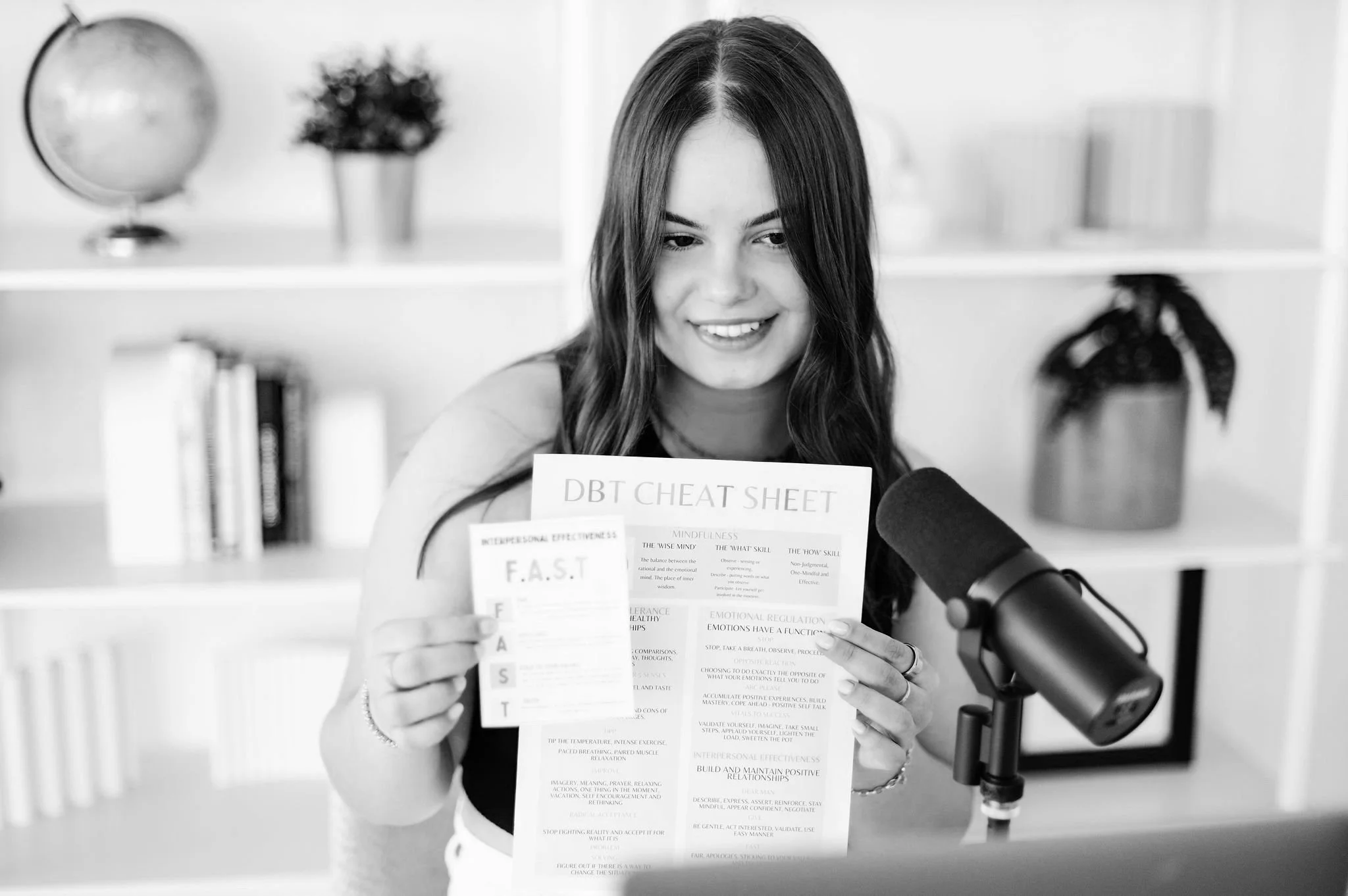
About She Persisted (formerly Nevertheless, She Persisted)
After a year and a half of intensive treatment for severe depression and anxiety, 18-year-old Sadie recounts her journey by interviewing family members, professionals, and fellow teens to offer self-improvement tips, DBT education, and personal experiences. She Persisted is the reminder that someone else has been there too and your inspiration to live your life worth living.
a note: this is an automated transcription so please ignore any accidental misspellings!
Sadie: Welcome to She Persisted. I'm your host, Sadie Sutton, a 19 year old from the Bay Area studying psychology at the University of Penn. She Persisted is the Teen Mental Health Podcast made for teenagers by a teen. In each episode, I'll bring you authentic, accessible, and relatable conversations about every aspect of mental wellness.
You can expect evidence-based, teen approved resources, coping skills, including lots of D B T insights and education in. Each piece of content you consume, she persisted, Offers you a safe space to feel validated and understood in your struggle, while encouraging you to take ownership of your journey and build your life worth living.
So let's dive in this week on She persisted.
Dr. Caroline: what I can tell you about isolation is, , it's the crux of all human suffering. And oftentimes individuals don't know how to have strong, healthy interpersonal relationships because it was never modeled for them on how they should do that. And repair takes a lot of vulnerability. It takes a lot of patience. It takes a lot of sitting down and talking through what triggered you, what hurt, how it hurt, and these are things that our society has no real interest in putting energy and time into
Sadie: Hello, hello and welcome back to She Persisted. I'm so excited you're here. We're having a really interesting conversation today with Dr. Caroline Fenal from Charlie Health, we are talking all things teen mental health, and especially loneliness and isolation because those are two of the most common things that teens struggle with at some point, and that can be really closely linked to other mental health challenges like depression and anxiety.
If you are not familiar with Dr. Caroline Fenal, she's a leader in adolescent mental healthcare. She oversees all aspects of Charlie Health's clinical programming, including the delivery of evidence-based care by teams of expert therapists. She's over 15 years of experience in evidence-based mental healthcare, including direct clinical experience working with youth and families across all levels of therapeutic care, ranging from residential to outpatient treatment. So obviously Dr. Fenal is very tapped into the team mental health space.
She interacts with individuals that are currently in actively struggling Extremely frequently, and that is why I'm so excited to have her on the podcast to pick her brain on ways that you can improve your mental health, what she's seeing with regard to trends in teen mental health care, and also ways that you can improve and support someone that is struggling with both loneliness and isolation.
So with that, I really hope you enjoy this conversation. As always, if you do, make sure to leave a review or share with a friend or family member. And if you post on social media and tag at She Persisted podcast, I'll repost and give you a little shout out. So, so excited to have Dr. Funko on the podcast today and let's dive into this convo.
Well, thank you so much for joining me today on the podcast. Caroline, I'm so excited to have you here on Supered and to dive into all things team mental health and treatment and loneliness.
Dr. Caroline: I appreciate you having me here and discussing this really important topic.
Sadie: I. Of course.
So to get started, I wanted to give listeners a little bit of context to how you got to where you are today Working with teens, , and having a lot of experience with outpatient treatment, teen mental health treatment, both in the context of working with teens and also their families. 'cause we do have a lot of parents that listen in wanting to help their teens, wanting to support them in this journey.
So how did you get to where you are today? , working with Charlie Health?
Dr. Caroline: Yeah. , it's, it's a long story, , but I'll try and keep it as quick as possible. , my story starts out in the suburbs of Philadelphia. I grew up as a kid. , struggling pretty significantly with some learning disabilities. So by kindergarten, , a teacher there identified that I had some issues around learning how to draw.
, from there, by second grade, I had done a battery of testing that showed. That I had dyslexia and I was also diagnosed at that time with a D H D, , and put on medications, which was very common in the, , early nineties to put seven year olds onto medication. , from there I went to a special school and, , For a school, basically for individuals who have those types of learning disabilities, who are neurodivergent.
And from there I went to high school and in high school, , got introduced to drugs and alcohol and I had a lot of feelings of being lonely throughout growing up. I have, , six half brothers and sisters that are all between 10 and 20 years older than me, so grew up. Feeling really alone. Didn't have any siblings, didn't have any real friends since I was, you know, neurodivergent different, , frequently did not feel connected to other.
Individuals. , by the time that I got to high school and went to my first party, I felt a feeling of belongingness that I had never felt before. And I always sort of felt like a round peg in a square hole. , but by the time that I got to high school and experienced, , alcohol use, a drug use, , suddenly I felt like I, I found my square hole, , and felt like I fit in from there.
Struggled pretty significantly with substance use issues. Landed in a D u I crashed and totaled my car and ended up in treatment at 19. , while I was in treatment, I was able to sort of see from the inside out what works and what doesn't work. , and especially being able to see what it looks like when it comes to isolation.
, you know, specifically felt. Really out of place in different treatment programs, which I'm happy to go into later. , and then once I found my tribe, my individuals who were similar to me, who looked like me, who sounded like me, who went through similar experiences, I felt like maybe I could do this whole sobriety thing.
, so got sober and , from there ended up. Going to school and, , took a couples and family counseling class as an elective. Thought that it'll be an easy course since, you know, I had all sorts of family issues and took that class. And then just fell in love with the professor. I think a lot of my, my career, my life is owed to the teachers that I had who really believed in me and the teachers that, , throughout my time in lower school, middle school, high school, , graduate school, who really took the time with me and so followed her, took every single class, suddenly had him.
A minor in it. Went and got my master's later, got my doctorate. , I met Carter, our c e o and co-founder when I was in an intensive outpatient treatment program when I stepped down from a residential program for the substance use issues. And, , Carter had given me a call and basically said, will you join me at, at another company that she was, , at the time.
With and asked if I could join to help with a startup. So, , fell in love with the startup world of helping teenagers that were similar to me. And from there, Carter and I, , came up with this idea around virtual treatment, allowing for access to every individual I. Who doesn't have access to high intensity therapy, accelerated treatment, multiple time a week treatment.
Those that are in crisis are suicidal. , be able to give that to them in their own home. And we started Charlie Health about three years ago, and today we've treated tens of thousands of patients and we're live in 25 states, , in just a few years, , which just shows us exactly how high the need was for a resource like this one that. Allows individuals to get multiple time a week therapy in the comfort of their own home when they're in crisis, when they're stepping down from an inpatient or residential program, when they're seeing an outpatient therapist once a week, who knows that they need something more.
, Charlie Health is there to fill the gap.
Sadie: I love that. And it's absolutely incredible and so necessary because there are so many barriers to treatment. Even just logistically, I remember my parents and I trying to make the decision of like, can I do this over the summer? Do I have to miss school to be able to get treatment?
Yeah, and for many, it's a decision of like is it bad enough that you have to take the step away from these larger goals, or can you. Do less intensive options and hope that works even if they're not as quote unquote effective. And that's what I wanted to ask you about is evidence-based treatments and evidence-based therapy.
Because there's a lot of discrepancies in the adolescent treatment world about different types of therapy and what's effective and what's evidence-based and what's not. So for listeners that are coming into this pretty much blind and they're like, I know I need therapy. I know I need support. What is an evidence-based treatment and how is that different from like, I'm gonna try meditating for a week and maybe that will help my depression.
Dr. Caroline: Yeah. you know, I think that oftentimes when we're talking to listeners, it always is something like, the answer is, it depends, right? Because everybody's an own individual and it depends on what it is that they're struggling with. What I can tell you is, , the idea of I have severe depression, I'm thinking about self-harming.
I'm gonna try, mindfulness for a week isn't gonna work, right? Yeah. , ideally it would work. If it did, we wouldn't have an entire mental health treatment industry. Right. , because we know, by the way, the evidence does show that mindfulness is an incredible tool when it comes to treating those that are struggling with racing thoughts.
Those that are struggling with feeling unsettled, those that are struggling with anxiety, mindfulness is incredible. I. , but at the end of the day, the people who you should be relying on to determine what type of therapy that you need are the people who have masters and doctorates in the brain. It's funny, my son is, is four years old and, and he, I.
Says to me, mom, you're a doctor. Can you look at this booboo? And I say, and I'm like, well, I'm not that type of a doctor. What kind of doctor are you? I'm the doctor of the head in the head. And he's Oh, the head. Okay. Yeah. You know, when you feel sad, mommy helps those people that feel sad. Okay. , my therapist
Sadie: said this, so I.
Hilarious story where when her daughter gets upset and her dad tries to help out, she's like, I need mom. She's a feelings doctor. You are not a feelings doctor. She's like, what are you doing here? Like, I need the feelings doctor right now. Feelings doctor. It's so
Dr. Caroline: funny. Yeah. Yeah. So I, I think that that like every individual who's thinking to themselves, look, I'm struggling a little bit with.
You know, and by the way, you could be struggling a teeny bit with some test anxiety and you need to work on that, or maybe somebody close to you die that you need brief grief counseling to get through it. Or maybe you're struggling with something that's chronic. You had a major trauma when you were a kid and you're still struggling with.
Sleep issues and still struggling with chronic anxiety, whatever it is, big or small. Getting a true assessment from a head doctor is perhaps one of the most important parts of determining what next steps should be. , we know that. Individuals like me, who I've been trained and and individuals all across the country can very quickly pick up on what's happening and what you need, and then can recommend in a very clear way what your next treatment plan should be.
Yeah.
Sadie: One thing that I think is really interesting about when you kind of entered the mental health treatment space is that there's been this shift in. Higher rates of anxiety and depression and family dysfunction. And obviously this has been a trend for a while, but I think with Covid, the conversation has just been extremely amplified and we also see people being a lot more vulnerable about what they're experiencing.
The conversation is a lot more open. So what have you seen there with regard to when people are asking for help, how they're trying to access resources, and also just. Like a large picture of how teens are struggling because it has changed a lot, even in just the past, say, 15 years.
Dr. Caroline: Yeah. , I'll start with the first part, which is around accessibility.
And the fact that c O V was an incredible conduit to improve the stigma that we had around virtual treatment. , I did my dissertation on the use of technology in a therapeutic setting. So my idea, my dissertation, was to go out and create an app, like a mobile app, and have it track different things like your number of steps, your emotions, your weather, the moon, whatever it is, and be able to have that app sharing data with the therapist.
And I did focus groups to see whether or not this would be an app that therapists would use. So I sat down with them. This is right, this is 20 17, 20 18. , and I said, so what does everybody think about technology in a therapeutic setting? And every single individual in this focus group said, I. I hate doing FaceTime sessions.
I hate doing Zoom sessions. It's the worst. I can't see my clients, you know, I can't see their, their body language and I can't see them eye to eye and I'm not breathing the same, you know, air as them. And that's the big difference. And you know, they just went horrible towards virtual treatment. And, , by the way, the research shows us that the research shows us that prior to the pandemic therapists, providers, Whether it be MDs, therapists, nurses, anybody.
Ha like really there was a big stigma against telehealth and that. Patients, people who really needed it love telehealth because guess what? They didn't have to leave their house. Get into the car, show up. Sit in a waiting room. Sit in a sterile room where you have an uncomfortable seat with fluorescent light coming in on you.
I mean, come on. You know, machine listening to the Wants to talk about, yeah. Yeah. Listening to the noise machine. Listening to the person. Fighting in the other room, right? Who wants to talk about their feelings, you know? And so there was this really big mismatch that happened and, and Covid hit. And suddenly all of the therapists recognized that if they're gonna have a job, they better, , get with the times and get on to virtual treatment.
And if they wanna help other people, they better do that. , And what we have found since then, and by the way, I'm, I'm still friends with individuals who were in those focus groups. They don't have offices anymore. They, they come to me and they're like, I can't believe that. During that time I was so against telehealth.
Now, I love it. My clients open up to me more often because they're sitting in their own home petting their cat, which makes 'em feel regulated. And suddenly now they're talking to me about things and trauma and things that they never thought that they would open up to anybody about. And they're doing it with me virtually.
And, , you know, I think that Covid really pushed us over that edge. It was that tipping point and it was, it was crucial. Or else we probably would've gone another decade with still doing in-person therapy. And then the worst part is not providing it to the people who are sitting in rural areas. Right who are an hour away from their nearest emergency room, , from the people who are in urban areas that don't have access to, to public transportation, to go to a therapist's office.
, you know, and then you have therapists that live in the middle of nowhere and don't have jobs. So, I mean, it just, it's suddenly improves access so incredibly to be able to provide it virtually. So that's something that we've definitely seen a lot of when it comes to how Covid impacted. Accessibility.
Sadie: I love that. And I, when you gave those examples, what comes to mind is a teen whose parents can't drive them to therapy multiple times a week and don't have time in their schedule. Correct. Or it's not logistically possible. And so to make those options available virtually is a complete game changer.
And I think is helping so many teens, which is really incredible 'cause you're in that awkward. Place of like not having enough autonomy to maybe access those resources and still needing that extra support of your parent, which can be amazing if you're not the one that's ready to advocate quite yet.
But they're the ones that are like, this teen needs help. What can we do? , so shifting gears a little bit to talking about loneliness and isolation, because it's something that a lot of teams struggle with and I think based on how we approach. mental health as a society and especially mental illness, we don't always think of those as mental health challenges or even something that might impact your mental health, and yet they definitely can impact and cause some of these symptoms, whether it's not feeling motivated to go out and do things that you typically would've enjoyed in the past or having low energy or having a lot of anxiety and rumination about social interaction.
So one thing that I think is really interesting is how. Loneliness and isolation can impact both physical health and mental health. So for listeners that maybe aren't familiar with that information and research, how can you explain what loneliness is, how it's defined, and then now how it impacts individuals?
Dr. Caroline: Yeah. , I. So I'm glad that you talked about the physical aspect of things, that it's really important. The , American Cardiatric Association came out around heart disease and was looking at this idea of mortality and, and rates around that. And what they found was individuals who reported feelings of loneliness.
, had a higher rate of heart disease. And then they also looked at it both subjective and objective. Right? And then it was like, do you live alone? And those that live alone have a higher rate of heart disease. So we always talk about this idea of dying of a broken heart. And you know, the, you, you married somebody, you've been with them for a long time, they die.
That's actually a real thing. , feeling connected to other people is something that helps our bodies. , oxytocin is a hormone that gets released when we're hugging somebody. , and these are things that are very, very important for our wellbeing, our physical wellbeing. you know what I can tell you about isolation is, , it's the crux of all human suffering. And oftentimes individuals don't know how to have strong, healthy interpersonal relationships because it was never modeled for them on how they should do that. So oftentimes families have a mom and a dad who are perhaps fighting, or siblings that are fighting.
And just not handling conflict in a really healthy way by repairing a rupture that happened. And rupture and repair takes a lot of vulnerability. It takes a lot of patience. It takes a lot of sitting down and talking through what triggered you, what hurt, how it hurt, and these are things that our society has no real interest in putting like energy and time into.
So what happens is you have a family that's filled with dynamics that are around being passive aggressive or just aggressive, , not working through these core issues that are going on. And then they go out into the world and then continue to have these unhealthy relationships with their peers and with their friends.
And the more that they have these relationships that feel really triggering, the more likely that they are to withdraw from another individual. And the problem there is when you withdraw from another individual, you usually withdraw from almost everyone. And when you do that, you no longer have those really good, feel good hormones naturally, and you seek them somewhere else, right?
, Brene Brown's always talking about the banana nut muffin and a, and a beer, right? This idea of trying to numb out those feelings of loneliness. And that's usually what is happening when it comes to individuals that are struggling with loneliness is, is this idea that they've never truly seen healthy relationships, and so they don't know how to be in healthy relationships, and the cycle just continues.
Sadie: You mentioned subjective versus objective loneliness. Is there a lot of denial and confusion that people experience about the phenomenon of loneliness? They're like, oh, I'm stressed, or, I'm too busy, or I'm not lonely. I have friends or family members. Is that common or are people really accepting of like, I'm lonely and that's what's going on for me?
Dr. Caroline: You know, it's a, it's a great question and I think that it's one that, , therapists. , especially with new and emerging research, have been spending a lot of time thinking about, which is, is this person acutely depressed? I. I e they have some kind of a chemical imbalance, , and they need medication and they need some kind of behavioral therapy around sleep hygiene and being better at sleep and being better at showing up to work and things like that.
Or is this something that's relational that's going on where maybe if they had a couple friends that they felt like they could rely on, that they felt seen and heard by, that could validate their experience. Their depression would go away. So it's like the chicken or the egg idea, right. Which is like, is this person lonely and that's what's causing the depression?
Or is the depression causing the loneliness? 'cause they're pushing people away because of the depression. , and it becomes this pretty intense cycle. And I think that's sort of the beauty of, of Charlie Health and, and group therapy in general, which is that we put individuals with other clients who look and sound like one another.
So that way they feel seen, they feel heard, they feel validated. They hear the words. Me too. I know what that's like. I've been there. And for them, once those feelings of oxytocin and feeling like they're being related to starts to fill up their own cup, the depression starts to seep away a little bit.
Mm-hmm. And that for us is, is the beauty of the connection, part of, of the therapeutic, you know, value that we provide for our clients.
Sadie: Yeah. You mentioned, , symptoms of depression and then also the hormonal changes that take place. Are there other thoughts or emotions or behaviors that are really distinct to feeling lonely and being isolated long-term that listeners can listen for and be aware of, whether it's in themselves or a friend, a loved one, et cetera?
Dr. Caroline: Yeah. , so I think we can look at two different things, right? We can look at what are you seeing in a friend, , just objectively like what are you seeing? And then more what are you hearing from them? So what are you seeing from them? This is a person who, when they feel feelings of loneliness, which is likely it's some kind of a mental health issue, it's leading to some kind of a mental health issue.
So these are gonna be individuals who might make plans and then might flake out on them. But look, people flake all the time, but I'm talking about chronic. like happening over and over again. , these are also going to be individuals who don't go to work or don't go to, , school because they're struggling so much with their anxiety and their isolation.
, this is also gonna be individuals who oftentimes you are Snapchatting them or whatever it might be, and they're laying in their bed. , and they spend a lot of time in their room, not necessarily outside with friends, , going to the movies, things like that. , and then this is also gonna be an individual who, , may self-harm in some capacity.
And when I say self-harm, what I mean is, , both, you know, cutting themselves as well as burning themselves, as well as even things like using substances. , and harming themselves with substances. , so those are some of the things you might see as far as what you hear. If somebody's struggling with these feelings of loneliness, you hear a lot of, I just don't know what to do, I just can't get out of it.
I just can't snap out of it. I feel like there's nobody that can help me. I feel like nobody understands me. There's nothing that I can really do to try and work through this. So a lot of feelings of both hopelessness and helplessness. Are oftentimes like signs that this is a person that's really struggling with isolation and and loneliness.
You
Sadie: mentioned that people will be struggling with loneliness and yet continue to avoid the things that might help, like going to work or spending time with friends. How do you kind of cross that bridge or close that gap between feeling really helpless and hopeless, but also not wanting to engage in the things that might make you feel better?
Dr. Caroline: , I think that that's the question of the, the human psyche. Yeah. Right. Which is like all of us know the things that are gonna make us feel better and yet we don't do them. And one could say we choose not to do them. One could say that we simply don't have the capacity to do them at that time. One could say that we feel too triggered to do them.
, one could say that we're not resourced enough to do them. , and so I think that everything is, is gonna be dependent on the person, so, mm-hmm. , for somebody like me, , When I am in my bag. That's what the kids use when you're in your depression bag. What do they call it now? I've heard that.
Sadie: Oh yeah.
Bed rott. I've heard that one. I've never heard in your bag. Okay.
Dr. Caroline: Okay. In your bag. That was, that was a thing like a couple years ago, so I don't know if it's still a thing, but,
Sadie: , I missed all the lingo. I haven't been in treatment in long. I know. I don't get any of these things anymore.
Dr. Caroline: I know well, bedrock you've heard of now, so yes.
All the news, if I'm in my bed, stories
Sadie: are freaking out about that at the moment.
Dr. Caroline: Yeah. We, we know that I have the capacity to get out of bed now, when I was 19 and detoxing did I have the capability to get out of bed? Definitely not. Like I just did not have the capacity to do it. Right. But now we know that like I'm professional and I can get outta bed.
So we know that I have the capacity to do it. Now the question is, do I have the motivation to do it? And the answer is yes or no. That depends on energy and how well that I've taken care of myself and my body. Right? And then we also have to ask ourselves, you know, I. Do I have the resources to do it?
I e do I have a loving person around me who could be like, come on honey, let's get out of bed. You know? Or like, do I have, , my dog who's like, you know, barking at me to take him out? Right? That's, that's the resources around you that you can have to rely on. , and so I think that a lot of, of this kind of comes down to, again, like where they're at.
Of whether or not they can make that change of, like, I know that if I get out of bed, I'm gonna feel better. I know that this will help me to feel less depressed or less anxious. , and I just can't do it. And when, when we analyze that can't, there's so many different reasons why they can't. And sometimes it really is they don't have the capacity.
And other times it's about resources and other times it's about. All sorts of other things, right? A medication change. There's so many different variables. One could argue that it's about your past lifetime, like on this day and three lifetimes ago, or I'm just saying like that there's a lot of different ways that we can think through why people don't take action when they're feeling those types of feelings.
, yeah, and it's a therapist's job, like it's the professional's job to figure that out and figure out what works for them. To
Sadie: put those resources and almost like that foundation in place. If someone is like, I don't have the support of friend, I'm not feeling motivated, the resources aren't there. What is your first step that you recommend people take?
Is it making an appointment with a psychiatrist? Is it reaching out to a therapist? Is it looping in that friend to be that caring person that's checking in? What is a good first place to start and then build upon with these other elements that can be supportive?
Dr. Caroline: Yeah, I think that there's two, two things that need to happen.
One is, , you need to choose an individual in your life that's a healthy individual that can hold you accountable and you need to call, you know, the back of your insurance card and, , get resources for a therapist to get in for an assessment. Not necessarily a psychiatrist. A therapist is really a good start.
and then make sure that that individual holds you accountable to show up to the appointment and helps you to make it happen.
Sadie: One thing that I think is really interesting that you have insight and expertise on is how this like situation or symptom or challenge, whatever you wanna describe it as, can impact a family as well, because while the teen might be the one that's struggling and feeling lonely, It also impacts the parents as they want to help and they don't know what they can do to be supportive and the teen isn't receptive to them telling them to get out of bed.
So how do you see things like loneliness and isolation impacting this like support group of friends and family members and other individuals?
Dr. Caroline: Yeah, so I mean the, the first thing to recognize is, Parent participation in treatment is the single largest indicator for positive outcomes. So parents have to be involved in treatment as much as possible, and by being involved in treatment, they're gonna feel a lot of feelings of shame and blame.
They're gonna feel like, and I'm, I'm sure that maybe your parents felt this way. I'm the reason why my kid is this way. Right? Like, I raised them this way because, you know, and I blame myself all day with my four year old. I mean, he acts like. Crazy. I'm just like, oh, obviously that's because yesterday I let him do this after he threw a tantrum.
So now he's throwing a tantrum again. And like he's doing that because I messed up the parenting yesterday. Like, parents are especially moms, right? Or like filled with mom guilt. And so when they show up to therapy and see that their kid is struggling, they oftentimes have some pretty significant emotional responses that are, you know, held in.
That aren't necessarily, you know, I'm a, I'm a therapist millennial, so I can talk about my mom guilt out loud, but a lot of moms won't and so, you know, oftentimes they feel an incredible amount of guilt. They feel an incredible amount of shame. , I think that Oprah Winfrey once said, , you're only as happy as your saddest child.
And I think that that's how a lot of parents feel when they think about. A kid that's struggling is, I'm only gonna be as happy as this kid. And so I better make sure , that she gets the help that she needs. , and then there's a lot of parents that come in that are incredibly defensive and are saying that it's all their kid's fault.
You know? And oftentimes that's you know, it's all your fault. You didn't do this, you didn't do this, you didn't do this. , you know, and you're a bratt and you're always on your phone and you take everything for granted, you know? , what is that underlying, that that defensiveness is, again, shame and blame.
Right. It's just directed differently. Yeah. Instead of directing it inwards, it's directed outwards. It's just a projection. , so oftentimes that's usually where the parents come in when it comes to their kids' struggling. , friends, I mean, friends are really tough, right? Because we talk a lot about this idea of.
you know, suicide becoming contagious in some capacity. So friends oftentimes can trigger one another. And it's really important when a friend is sharing a trauma or sharing what's going on, that they do this in a safe place and that they ask the friend like, are you okay for hearing this? And that's why, you know, group therapy is so beautiful 'cause you're doing it in this really contained setting with a therapist that's present, so that way they're not triggering one another all over.
Yeah. , Yeah,
Sadie: I think that's really important. I think it's something that teams can struggle with a lot is kind of having that separation between what can I talk to with my friends and have it be effective and what can cause more challenges within the friendship. , and depending on what you're sharing, that can be really hard because then you get into the thought process of, well, If I'm talking about this, does this make me a burden?
And it's kind of making that differentiation that, well, you can go to your friends, ask for support, but your friends also can't take on the role of a therapist or take on the role of your peers in group therapy. And so it's understanding that audience and making sure that need is getting met.
If you do need to talk about those things with your peers or with a professional, I wanna end on how teens can increase connectedness, increase independence. We talked a lot about how to address loneliness and isolation and how that impacts everyone around the person that's feeling really lonely and isolated.
But what are your tips and pieces of advice for teens that that wanna be more connected and. Have that independence and set themselves up for success as they go to college and are really stepping into that, , era of life where they're very much in charge of their mental health and there are less, , things in place to keep them on track with regard to physical and
Dr. Caroline: mental health.
I mean, so I'll say this time and time again, I feel like I say this in every, every speaking engagement that I have, which is. You know, teenagers need to find their passion. They have to find what they love, what do they love? And by the way, they can love a million things. That's fine. Right? And if they don't love one thing, , that's okay too.
Don't shame yourself 'cause you don't, but. At the end of the day, my love is animals. So I get out of bed because I need to go and feed my mini donkey. , that's why I get out of bed every day. It's not that way. I can go help thousands of teens. It's not that way. I can go and see my four year old toddler, that's why I get out bed.
, and you know, teenagers oftentimes come. Usually at age 9, 10, 11 with something that they love, be it poetry, art, writing, music, whatever it is. And I always say, you know, utilize that passion that they have. Sports, for example, to get them out. And with other people that also love that that activity, that is just a huge way to help them to connect to others.
And it's easy, it's like low hanging fruit, right? We don't have to get them like into a volley, like they've never played volleyball because you gotta get them to a volleyball thing. That way they can meet friends of all. No. What did you used to love when you were a kid? You know? And then you, I have a kid said to me once, you know, I loved bugs.
You loved bugs. Tell me more. I used to love staring at bugs. Playing with bugs. Okay. Type in bug center. I found this person who, who was near us, that was in a high school that studies bugs and I set them up with one another and now he's studying bugs at the school that he is going to. Okay. That's hilarious.
Entomology is what it's called, you know, so it's like you, you have to focus with teens and young adults about what it is that makes them jazz. Other than TikTok and like their phones, right? Because that's like the thing, right? But you know, other than that, what gets them excited, what gets 'em jazz, and then find other individuals who can help them around that and who they can then relate to.
That's a huge, huge part of this. , and then I think too, in addition to that, you know, When you spend time, one of the big things that's really helpful is when a kid, , doesn't wanna hang out with friends and wants to cancel and wants to cancel and wants to cancel and then shows up and then they're just like honest about it and they're like, yeah, I was really gonna cancel coming out tonight.
Like I really, I wish that we didn't do that. You're just honest. You will find that the four other people's like, dude, I also really to cancel tonight. Shame. That you felt like around wanting to cancel and not being there, but then finding out that everybody else wanted to cancel too, really oftentimes can lift a huge burden and help with your anxiety by just talking about it and being vulnerable and discussing like the fact that, you know, I wanted to just lay in bed and watch TikTok and like, Sometimes I'll say to my friends, I'll be like, can we just like hang out side by side and just scroll on our phones?
You know? But that does help. , and in my brain I'm like, I don't want to hang out with a person right now. Like, 'cause whenever I think about the stress of hanging out with them, I'm thinking about how I'm gonna be drained and how it's gonna be hard. I don't wanna start conversation. So sometimes I'll just say to my friends, can we just sit next to each other and just scroll on our phones?
But then we're like, look at this meme, look at this. And then you're talking and you're suddenly not isolated. Right? Yeah. , so being able to lower those expectations is also really important.
Sadie: Mm-hmm. Where can listeners access Charlie Health as a resource and continue to follow along with all of your amazing work?
I.
Dr. Caroline: Yeah. , so listeners can , go to charlie health.com and they can also look up our Instagram, which is at Charlie Health. We have a TikTok at Charlie Health. I have my own Instagram, Dr. C L C S W. , and yeah, they'll be able to get a lot of resources through all of those different types of ways. And of course, they can always call our admissions.
Our admissions are open 24 7. We're here to help. , we can get clients in within 24 hours. We really specialize in clients that are in crisis. So, , individuals that are, you know, maybe not safe or need something more intensive than once a week therapy, we can get them in pretty quickly. 'cause that's our, that's our mission.
Amazing.
Sadie: And that's so important. I know from firsthand experience when you are in crisis and you need a a provider and you're going through the process of like onboarding and getting to know someone new and being diagnosed, it can be really challenging. So I'm really happy to hear that you guys are filling that gap in the market and helping so many teens that need it.
Dr. Caroline: Thank you for everything that you are doing. Oh, oh, thank you. We need individuals that are young, that lead with lived experience of this and. I'm really impressed with everything that you've done, so
Sadie: thank you. And thank you so much for coming on today.
Thank you so much for listening to this week's episode of she persisted. If you enjoyed, make sure to share with a friend or family member, it really helps out the podcast. And if you haven't already leave a review on apple podcasts or Spotify, you can also make sure to follow along at actually persisted podcast on both Instagram and Tik TOK, and check out all the bonus resources, content and information on my website.
She persisted podcast.com. Thanks for supporting. Keep persisting and I'll see you next week.
© 2020 She Persisted LLC. This podcast is copyrighted subject matter owned by She Persisted LLC and She Persisted LLC reserves all rights in and to the podcast. Any use without She Persisted LLC’s express prior written consent is prohibited.