183. High-Functioning Depression & Trauma in College Students feat. Judith Joseph, M.D., M.B.A.
listen to this episode:
Tune in and subscribe on your favorite platform: Apple Podcasts | Spotify | Stitcher | Google Play | Radio Public | PocketCasts | Overcast | Breaker | Anchor
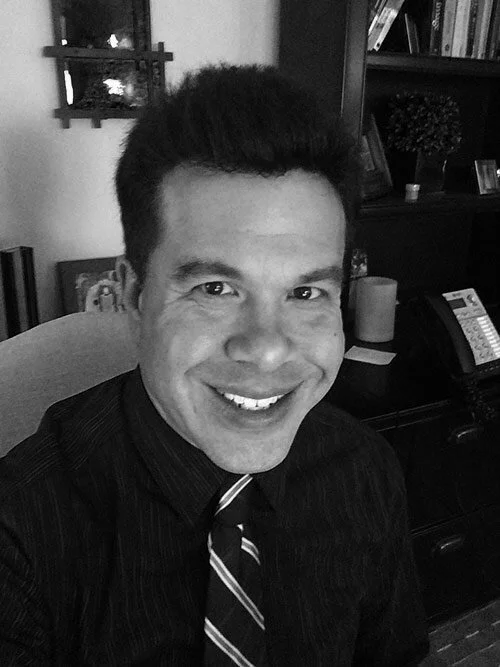
Today's guest is Judith Joseph, M.D., M.B.A.— a board-certified psychiatrist and researcher, Chair of Women in Medicine at Columbia University Vagelos College of Physicians and Surgeons, Clinical Assistant Professor at NYU Langone Medical Center, and founder of the first research lab to study high-functioning mental health conditions. She posts social media content for over 1 million followers and recently received a Congressional Proclamation from the U.S. House of Representatives for her social media advocacy and research.
In this episode, we discuss:
+ Why high-functioning mental health disorders can be overlooked
+ Signs someone has high-functioning depression
+ What scarcity trauma is and why someone may be experiencing it
+ Overlaps between high-functioning depression & perfectionism
+ Red flags that a student is struggling with high-functioning depression
+ How high-functioning depression can affect relationships
+ The keys to preventing & overcoming high-functioning depression
+ Her research on sexual trauma & domestic violence in college
+ The two main things trauma survivors need in order to heal
+ How sexual trauma look different in college compared to other environments
+ Advice she wishes all college students could know
+ so much more!
Dr. Joseph's Instagram: https://www.instagram.com/drjudithjoseph/
Mentioned In The Episode…
SHOP GUEST RECOMMENDATIONS: https://amzn.to/3A69GOC
STARBUCKS GIFTCARD GIVEAWAY
Want coffee on me?! Each month I'll be randomly choosing a winner to receive a Starbucks giftcard! To enter this giveaway, all you have to do is leave a review of the podcast on Spotify and/or Apple Podcasts and DM me on a screenshot of your review on Instagram. Win bonus entries by tagging the podcast on your Instagram story or TikTok! Good luck!
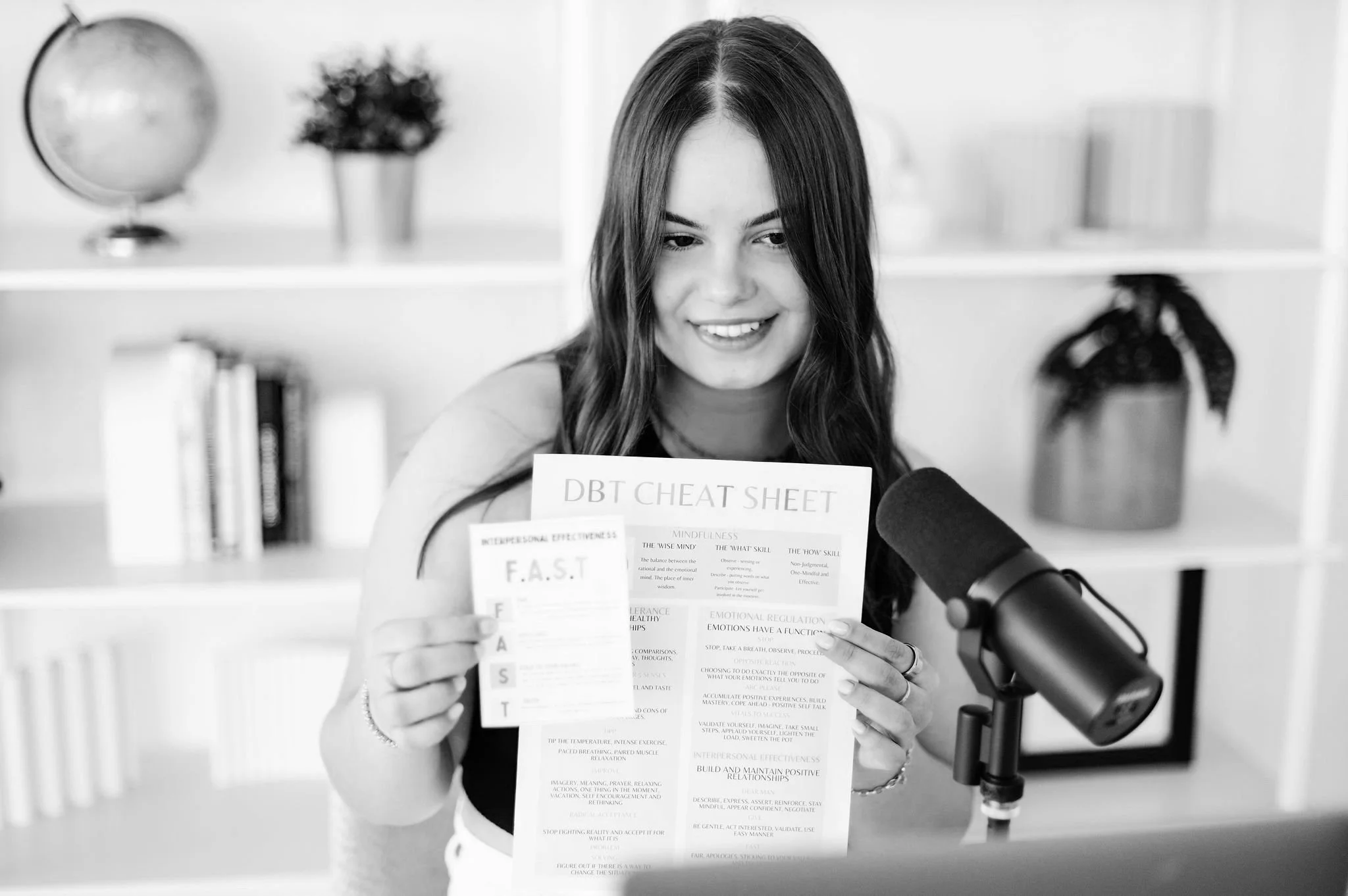
About She Persisted (formerly Nevertheless, She Persisted)
After a year and a half of intensive treatment for severe depression and anxiety, 18-year-old Sadie recounts her journey by interviewing family members, professionals, and fellow teens to offer self-improvement tips, DBT education, and personal experiences. She Persisted is the reminder that someone else has been there too and your inspiration to live your life worth living.
a note: this is an automated transcription so please ignore any accidental misspellings!
Sadie: Welcome to She Persisted. I'm your host, Sadie Sutton, a 19 year old from the Bay Area studying psychology at the University of Penn. She Persisted is the Teen Mental Health Podcast made for teenagers by a teen. In each episode, I'll bring you authentic, accessible, and relatable conversations about every aspect of mental wellness.
You can expect evidence-based, teen approved resources, coping skills, including lots of D B T insights and education in. Each piece of content you consume, she persisted, Offers you a safe space to feel validated and understood in your struggle, while encouraging you to take ownership of your journey and build your life worth living.
So let's dive in this week on She persisted.
Dr. Judith Joseph: I see people delaying gratification in the sense like, when I finally get into this school, I'll be happy. Or when I finally meet the love of my life, I'll be fulfilled. But these type of individuals they never feel satisfied.
They're never satiated. It's always onto the next thing. Like, okay, I got this job, but then I got to get the promotion, but no, not just the promotion, then I got to get the house, you know, and then you find yourself working, working, working, working, and not really feeling satisfied. And you just have this mindset, , that you just can't ever relax because then, if you relax, you may lose everything,
Hello, hello, and welcome back to another episode of She Persisted. I am so excited you guys are here today. We're talking about such an important topic that I'm sure is going to be really of interest to all you guys. We're talking about high functioning depression and trauma in college students. We have Dr.
Judith Joseph on the podcast today. She is a board certified psychiatrist and researcher, the chair of women in medicine at Columbia University. She is a clinical assistant professor at NYU, and the founder of the first research lab to study high functioning mental health conditions.
So fascinating, was so excited for this conversation. You might also recognize her because she is super active on social media with a following of over 1 million individuals. So And she recently received a congressional proclamation from the U. S. House of Representatives for Social Media Advocacy and Research, so she has such an incredible career and so much expertise to give us in this area, and I know you guys are going to love this conversation. We talk about high functioning mental health disorders and why they're often overlooked, signs of high functioning depression, scarcity, trauma, and why individuals experience that, overlaps between high functioning depression and perfectionism, read further.
flags that students are struggling with high functioning depression, how that can impact relationships, the key to preventing and overcoming high functioning depression. We talk about research on sexual trauma and domestic violence in college, so a trigger warning, for that area of research. We also talk about the two main things that trauma survivors need in order to heal.
And also sexual trauma in college environments versus other contexts, which is super interesting. And then we wrap up with advice that Dr. Joseph wishes that all students could hear and know going into that experience. So, such an incredible episode. I learned so much. I loved getting to pick Dr.
Joseph's brain about all these incredible topics, and this is so relevant to individuals that are going to be going to college or actively in college or parents of college students, so I really hope you guys enjoy this episode. As always, if you enjoy, leave a review, share with a friend or family member, and we do a Starbucks gift card giveaway every month, so if you want a coffee on me, all you have to do is leave a review, send me a screenshot on Instagram, email, whatever is easiest, and you will be entered to win.
So, I hope you guys enjoy this episode and enter the giveaway, and I will talk to you next week for a solo episode.
Sadie: Well,
thank you so much for joining me today. I'm so I'm so excited to have you on She Persisted.
I have been following you on social media for a while and I love your content and I'm so excited to dive into all the different areas that you research, all of the different , areas that you share on social media about the clinical population you work with and I'm just really excited to have you on the show.
Dr. Judith Joseph: Thanks for having me. I'm excited to be here. And I'm glad that we're talking about high functioning depression too, because students, especially at Ivy League schools, right? You see it everywhere. Yeah, I think it's very relevant.
Sadie: It's crazy. 100 percent It's so interesting at Penn, they Every single student knows of this thing called Pen Face, like the teachers know about it, the counselors know about it.
And it's everyone like pretending to be fine and internally struggling and not talking about it. And it's just like universally accepted. I'm like, guys, this is not a great, we got to do something here because this is not effective.
Dr. Judith Joseph: It's accepted because like it's normalized and when people who walk around on campus have it, you're Your teachers have it, your professors have it, your research, , lab assistants have it.
If it's everywhere, then it becomes something that, well, what makes you special to get treatment, right? Like, you know, if it's just so common, why even talk about it? Which is a huge misconception.
Sadie: 100 percent. Before we dive into all of that, I would love to get your background and how you landed in this different space in the mental health field because you were one of the first individuals to really study high functioning depression and you also have a lot of other areas that you have done research on.
How did you decide to start focusing on this area? What brought you to this kind of area of research?
Dr. Judith Joseph: So I'm a psychiatrist, which means that like I can treat patients with like therapy and medication. But when I first went to medical school, I never thought that I would ever be in mental health.
I was like, you know, I'm going to be in the operating room. And I actually did anesthesiology for like two years in residency. And then I was feeling like, you know, this is a lot of work to get to a field that where I'm feeling either bored or very, very stressed because when you're in the operating room, you're either, , kind of like just monitoring a patient or you're trying to keep them alive, which is just too extreme for me.
And I just kind of felt myself feeling like, what did I do all this work for nothing? Like, you know, so I started thinking. About fields that actually, , felt purposeful to me. And I remember that when I was in medical school, I did this rotation in South Africa where I was working with orphans and doing trauma focused groups.
And I just remember feeling like, Oh my gosh, I'm making a difference here. And that was like the only time I felt really. , fulfilled. So I talked to my advisors and I was able to switch into a psychiatry program. But when I was entering psychiatry, I just felt like, well, there's nothing wrong with me.
Like, I don't have any mental health issues. That's like kind of something that other people have and I want to help them. But as I learned about it, I was like, oh my gosh, so many people, including myself, have mental health issues, but we just don't acknowledge them. And I think it's because we mask and also because our fields kind of normalize it.
Like when I was looking around my medical school class and my residence, and I was like, Oh my gosh, we're all stressed. We all push through our pain. We don't acknowledge our pain and we just mask it. You know, we keep going. And that really was the beginning of my interest in high functioning depression, but running my research lab, I was I recruit, I'm a principal investigator of my own research lab in Manhattan, and I recruit patients into depression studies.
And what I found over the course of the pandemic was that a lot of people were coming in, they were meeting criteria for certain parts of depression, but not fully meeting the full, you know, they weren't fitting into a box because they weren't low functioning. They weren't really acknowledging being significantly distressed.
So they weren't qualifying for these studies, but they were saying like, well, Dr. Judith, something's off. I just can't put my finger on it. So I thought, okay, let me just put out a reel out there on social media. Cause I had just started working on social media and you know, let me see if anyone else feels this way.
Cause I'm seeing it so much in my research practice. And then my social media manager was like, you know, you got to open up your TikTok. This is going viral. And I was like, what? High function of depression? And she was right. Like, people kept being like, that's me. Do you have a camera watching me?
Like, how do you know my life? And I'm just like, oh my gosh, this is a thing, and I gotta figure out what this thing is. And that's what led me to my research.
Sadie: You mentioned a couple of things when you were kind of looking at the cutoff for the Full depression diagnosis, whether that's like major depressive disorder, maybe it's persistent, maybe it's seasonal.
What were those differences that you kind of saw on that spectrum of the depression diagnosis? You mentioned there wasn't that impairment, they maybe weren't low functioning, there wasn't as much distress, but what symptoms were you seeing that was like, okay, something's not right here, even if they're not meeting all the DSM criteria yet?
It
Dr. Judith Joseph: wasn't that they were not just not. low functioning. They were very high functioning. And what I was seeing was them keeping themselves really busy in an effort to unconsciously block whatever pain that was. Many of them don't even identify as it being pain. It's just something's off, but they can't describe it.
So what I think it is, is something prodromal, which means leading up to, but not necessarily fitting into a box. And that's why there's no diagnostic code for it. You know, you hear things Expert saying, oh, it doesn't really exist. Maybe people are talking about persistent depressive disorder or dysthymia But no like this doesn't cause an impairment and people are actually thriving.
They're killing it You know, they're the ones with the pen face walking around saying, you know, like getting good grades, showing up not showing anything In any way in the form of distress, but then we hear those stories where the person that, you know, we all knew and we would have thought of them as the last person in the world to do something that showed distress or to do something scary.
We find out that, you know what, this person was masking a lot of things and maybe they didn't even realize it. So, you know, if it becomes so normalized in a certain culture, in a group, then people don't identify it. And I think that a lot of experts in particular doctors don't identify it because a lot of them in health care.
probably have high function depression too, or some form of it. think about what people went through during the pandemic, working through all those conditions, being healthcare heroes. You're telling me that they don't have high function depression. I don't know. I think we have a case study there to begin with, but, , I do think that it's a public health crisis and I'm hoping that my research will lead to some sustainable solutions.
Sadie: Yeah. Anecdotally, and this would be, like, things people responded to your video with, or patients you've had conversations with, are there certain, like, common themes of thought patterns, or belief systems, or different emotions that they're experiencing really intensely? You mentioned this, like, extreme avoidance and throwing yourself into these other areas.
What were people talking about and sharing that kind of Raise those red flags that like, okay, you have high functioning depression.
Dr. Judith Joseph: Interestingly, I'm seeing a lot of scarcity trauma, and it's a term that a lot of therapists have never heard of. For example, if your therapist is from like an upper middle class, Or middle class background and you come from a position of poverty or, or, or lesser resources.
, or if your parents came from, , lesser resources and their scarcity, trauma and those behaviors trickled down to you. You may not necessarily talk about it with a therapist because A, you may be ashamed of your history of having limited resources. Maybe you were teased for it. Maybe you were ostracized for it.
Maybe you tried so hard to assimilate and blend in. That you just don't like to talk about it, and a lot of us who are in therapy don't necessarily want our therapist to not like us. You know, we like to please our therapist and we don't want to feel rejected and maybe conscious on the aware level or on the unconscious, subconscious, unaware level that we're doing this.
So we're not showing our full and complete selves to this therapist, and we're not sharing our scarcity trauma. And many of us aren't even aware of the scarcity trauma that we have. So I'm seeing a lot of people who were either immigrants or came from positions where they didn't have privilege, , feeling like they don't, they shouldn't complain.
You know, they have things other people don't. In their families or generations before them didn't have right or their families brought them up in a culture where you know, you don't really talk about your pain. You just push through your pain You push through your progress. You don't feel your emotion So I see a lot of that and I see people delaying gratification Not in the sense of the way that you learn it, you know in psychology courses where you know People who have delayed gratification have better outcomes.
It's a different type of
Sadie: study with the kids, right? Not the
Dr. Judith Joseph: marshmallow case study You But more of the, like, when I finally get into this school, I'll be happy. Or when I finally meet the love of my life, I'll be fulfilled. Or when I finally don't have students at, then I can like relax. But these type of individuals they never feel satisfied.
, they're never satiated. It's always onto the next thing. Like, okay, I got this job, but then I got to get the promotion, but no, not just the promotion, then I got to get the house, you know, and not just the house. I got to have the kid. And not just the kids, the kids got to be in this type of school and it just never ends.
And then you find yourself working, working, working, working, and not really feeling satisfied. And that type of culture trickles down to the next generation, right? So we're not all aware of this. And, , and a lot of people who come from. Families who, let's say, were refugees or left, , countries with limited resources or just, you know, just don't have resources or came from generations where there was something terrible that happened earlier in the generation pool and, like, you just have this mindset, , that you just can't ever relax because then, you know, if you relax, you may lose everything, then you don't realize how that, , you know, that really affects you.
And so I'm seeing that a lot. , in my research with, high function depression is that scarcity trauma.
Sadie: Do you see a lot of perfectionism and like perfectionist traits and styles of thinking in this population as well?
Dr. Judith Joseph: Yes, these individuals are not people who are easy on themselves. They tend to be the rocks.
And I'm not saying that all people with high function depression are Excelling or killing it and everything, but they do, they're hard on themselves, you know, , they tend to allow others to make mistakes and when they make mistakes or perceive mistakes, they're very very hard on themselves , you know, they they internalize a lot of guilt and shame And , so I do think that There's that perfectionistic quality to them, , not in this classic sense where we think of like perfect grades, perfect this, perfect everything, but they're just hard on themselves.
They don't allow themselves room for error. You know, if you, if you think about it, , these individuals, if they do one thing that they perceive as being, , And anyway, a shortcoming, they will replay it over and over again in their head. They may have dreams about it. , and they just, they don't allow themselves to get compassion a lot of the time.
So, so yes. And that, that overworking mentality can be. Overworking on yourself, you know, like you can not allow yourself to relax. , so I see that a lot.
Sadie: I would love to talk about how this shows up in different arenas. And you do a lot of great social media content about this kind of explaining the differences of how this can show up in relationships, in an academic setting, in work settings, in unhealthy relationships. Starting with students and being in that academic environment where, like you mentioned, there are a lot of these external markers of like, I want to get this grade, I want to do well in this area, I want to get into this school.
And when you have that, like, lack of self compassion, you're holding yourself to such a high standard. Academics can be a really great place to start. You have a tough relationship with that. So how do you see high functioning depression show up in students? And, , is it different from other areas and, like, demographics of
Dr. Judith Joseph: individuals?
I recently did a reel on this where a student isn't sleeping because they're having dreams or nightmares, actually, about depression. Failure, , and then, you know, getting good grades or getting a grade that they desired and then not taking the time to celebrate their wins and just onto the next project and then self medicating with alcohol, you know, binge drinking or using substances.
Because of the anxiety again, because they're hard on themselves, so they don't allow themselves to make any type of mistakes and social settings. , and also seeing that there's like this intensity about them, you know, like they crave a friendship. They don't want to be lonely, but at the same time.
They're so competitive that they don't want to share their notes. So like, you know, maybe they won't become friends with someone because they may have to study with that person and share a bit. So there's a lot of, there's a lot of intensity involved in these situations a lot, , with students. , and then you sometimes do see, , habits that are reflective of, , other types of depression, like not wanting to eat or eating too much.
maybe not really getting a lot of movement or just, you Taking it another level, you know, extremes are, are usually red flag. a lot of times if they do decide to exercise, they're all in, they're like in the gym, lifting the heaviest things after not, , lifting for, for months.
Right. So it's a lot of intense behaviors because there's very little self compassion. , so there's, there's little room for
Sadie: grace. Yeah. What about relationships? I mean, you've mentioned so many areas that self compassion is so closely correlated with this high functioning depression, and there's , that saying where it's like, you can only love others as much as you love yourself.
So I can only imagine how challenging it is to show up in relationships and have those healthy dynamics. When you are struggling with high functioning depression. So what have you seen anecdotally? , what have you heard from people on social media and all of that, when it comes to relationships?
Dr. Judith Joseph: Relationships are so complex. You know, I've seen a lot of different dynamics. One of the dynamics that I do reels on have to do with the fact that when you're so busy, , you're not really taking the time to vet people. So you end up in sometimes very unhealthy relationships because you're, you're You're too busy to actually find out if someone's right for you.
, and also we talked a lot about family dynamics and how, these scarcity, you know, Mindsets, these scarcity traumas trickle down. And so you may be accustomed to emotional scarcity where like a caregiver or a parent didn't really show a lot of love and tenderness and nurturing, because they were in that mindset of like, we could lose it all.
We got bigger things to worry about. So you're not accustomed to people being tender to you. So you may gravitate towards what is. familiar, and familiarity is not necessarily healthy, so you may, , end up in relationships that are not emotionally nurturing because that's what you're accustomed to. So, there are different dynamics, , involved with, with these individuals.
Sadie: I, am wondering if, thinking like 30, 000 feet level, 10, 20 years from now, do you think that if people truly acknowledged perfectly hidden depression and were aware of the warning signs and started asking for help and asking those resources at that point, do you think it would prevent some of these long term either or lifelong struggles with depression or a full blown major depressive disorder diagnosis down the line?
Dr. Judith Joseph: I do. I think that, you know, with early education, we start off in the right place these days. We spend a lot of time with face charts and emotion charts and children looking at charts and saying like, I feel pain. I feel depressed. Now, I think when I was in grade school, there were like 10 emotions and now they're all like a hundred, right?
Like, it's crazy. But I do, I do think that in certain circles We tend to move away from it. It's like, we start off in the right place. We teach kids that, it's important to feel, you got to listen to your body, you got to know when you have to go to the bathroom and eat and be hungry and need soothing.
But then when you become an adult, , it's like, well, stop thinking so much about your emotions and do stuff, ? And so a lot of us will sit through, you know, an entire exam holding our, our, you know, our urine, not pee, or we'll sit and, , study and like, And then like overeat at night.
You know, we don't listen to our bodies. We don't listen to our emotions. It's almost like the more higher level, , that we get in terms of our intelligence and our stature and our careers, less attuned we are to our emotions. And I think that, you know, if we, as a society and As human beings, really hold our emotions sacred and pay attention to our emotions and, , and protect them and, really revere them, then we can actually learn from ourselves and, and follow, , procedures and processes that are actually helpful for us and healthy for us.
But I do think we tend to regress, you know, as we get older in terms of our emotional intelligence because of capitalism and society and pressure to succeed. , so I think we do need to go back to the basics in
Sadie: many ways. Yeah, it's so interesting. It's like this cycle where, again, we start out in a really good spot and we're like, boundaries, ask people for permission, like, this is a healthy relationship.
And then you lose all of that. And then a lot of people lean so far into self help and learning all these things and trying to like, make up for all this lost time and learn these new ways of talking to themselves or being in relationships or just like, Having healthier habits, and it's like you're talking about, there's that period where we move so far away from like that healthy place of functioning and listening to what we're feeling and thinking, and it can cause so many problems.
Dr. Judith Joseph: It does. We really do stop listening to our bodies, and it doesn't make sense because our bodies carry us. through our entire lifespan. So, and our brains are, are a part of our bodies. So if we don't listen and honor this vehicle that, you know, we need, , then what, then where are we going to be?
It's not going to be a healthy play.
Sadie: A hundred percent. If you had some advice for individuals who have heard you describing high functioning depression and they're like, that's me, that's exactly what I'm experiencing. Maybe they listened to your podcast, they have followed you on Instagram and they're looking for some tips for how to start shifting some of those patterns, increasing that self compassion, giving themselves more grace.
How do you recommend that people kind I'll learn this way of functioning.
Dr. Judith Joseph: I think listening to your bodies is so important. It sounds like simple, but we really do have to go back to the basics. And remember, a lot of us are just pushing through life, not feeling, not acknowledging, and just hoping and holding our breath and hoping that it gets better.
It's not going to get better, you know? So in many ways, there's a lot of regression. It's the magical thinking that we had when we were toddlers. If I close my eyes, then. You can't see me. Not that like, Oh, like I can't see you. Yeah. Yeah. You can see me, but it's the same type of mentality. Like if we just like close our eyes and then hope for the best, it'll get better.
But no, we have to acknowledge it. We have to respect that how our body and our minds feel and honor that. And that's a good place to start, which is not easy. It sounds so granola, but it is so not easy. It's it can be very painful for people. And there are people in. Who are in treatment with me for years.
And they have to relearn how to like get back in touch with their bodies and their minds and their emotions. So, , but that's a good place for us all to start and mindfulness can be very, very helpful. It's an Eastern philosophy and it really teaches you to sit still, which many of us can't do. We can't just sit still.
, so start with that one minute a day. It sounds minute, no pun intended, but it really goes a long way if you can add those minutes up over time.
Sadie: I love that, and I think it's, again, we talk about the population that this advice is directed towards, and they're so busy, and they have so many things they're balancing.
They're like, this isn't a priority. So, , Making time for one minute of mindfulness is a very reasonable goal. It is something that you can take time to do, and like you're saying, it can have really profound impacts, especially if you keep working that muscle and continuing to build up that skill set with sitting in the present and paying attention to where your thoughts and feelings and emotions are and all of that.
Dr. Judith Joseph: And anyone can do mindfulness. I teach little children mindfulness. I use the Kung Fu Panda movie. , it's an old, like, I think Pixar movie and I play that snippet and they're like, I get it, you know, like, just like how you got it eventually. So I think we can all do it, but are we all capable of making time for this?
Right. And so is this something that you are.
Sadie: I want to shift gears a little bit to another area that you study and work on within a similar demographic of like college students, which is sexual trauma and domestic violence, which we haven't talked about much on the podcast before. We've done some episodes on trauma and healing after that, and PTSD.
and all of that, but I would love to understand your research there and your experience and what you're seeing, especially in the college demographic, because it is a very unique period in time. And like you're talking about, when we get away from these like resources and, , this habit of asking for help, especially in college, when you go through something like that, it can be so challenging to feel like other people get it and they've been there and there are resources out there.
So. What are you seeing? What is your experience there?
Dr. Judith Joseph: There's something that is inherent to, and I'm going to talk about women's mental health, because women, unfortunately, are, you know, the typical victims of sexual trauma. , and we know that this is not just old data. The CDC is reporting as recent as February 2023, that young girls.
Adolescents are experiencing a lot of trauma, sexual trauma. And, you know, these adolescents become college kids, right? They become college students. So it's a problem and internalized shame and blame is a hallmark. It's central to trauma. People have horrible experiences. And don't seek help because they're ashamed.
They think somehow they, they, you know, brought this on themselves. That they should have known better. That they should have been more alert. And I just, I can't emphasize that enough because it's actually a question on something called the Caps 5 which is the gold standard for, for PTSD assessments. It's actually one of the questions and it's actually one of the symptoms in the DSM 5, which is the Bible of psychiatry, internalized blame and shame.
So if you're walking around with that, know that this is a symptom of PTSD, blaming yourself and feeling shame are symptoms of the trauma. So there's nothing wrong with you. This is a symptom of the trauma, but I do think that's why a lot of people don't get help. , because that shame is just so prominent.
It's so overbearing at times. And also society does blame you. You know, like you will, you'll see that when you go into an ER or into any type of place where you are seeking treatment and support. Someone somewhere will blame you. Right? They may not be aware of it. , but you know, it's, it's sometimes unconscious, sometimes it's conscious, but just know that that's not right, that this is not your fault, that no matter what you did, you didn't deserve it.
And I always say that. , and I think that, , When you go through trauma, the first and foremost thing is know that it's not your fault, and then you have to feel safe. Do what it takes to feel safe. So if it means that you have to take a break, you know, that you need that safety and comfort and support from people, do what it takes to feel safe.
If it means that you have to get rid of, , temporarily or permanently relationships that are not supportive and healthy, do what it takes to feel safe. If it means that you have to go to a place to get treatment. , and, and you need physical safety, do what you have to do, you know, like, so safety is important and it's, so important because the data shows that if you can minimize the blame and shame, and then if you can increase the safety, right, if you can get out of that relationship, if it's a domestic violence or intimate partner relationship, or someone random, or, you know, someone that you knew, , if you can get away from that, and if you feel safe, you're, you're, , outcome, both long and short term, It's just exponentially better, right?
But if you don't, if those two factors aren't there, it's going to be harder for you. So safety and decreasing shame and blame are really, really important, for these, , populations for people who have survived trauma. And if you see something, don't ignore it. If you see it happening, if you see patterns where, you know, someone's being isolated, if someone's being, , , ridiculed and emotionally shamed, or if someone's trying to change them, you know, and don't ignore those signs because that person needs community and we heal this way.
We heal by helping others. We heal ourselves by helping others. So, so don't ignore it.
Sadie: Are there different ways that you see college students either approaching these situations or coping with them or maybe those different patterns and how they are accessing resources or even how they think about these type of dynamics or experiences?
It's really interesting because we all hear, or most of us have heard about, these the data about how high the rates of sexual trauma and rape and sexual assault are. I forget what it's called, but the period before Thanksgiving, a freshman year of college for girls. And there are incredibly high rates of assault and rape.
And I remember my parents being like, you need to be aware of this. Like, this is no joke. Every parent's worst nightmare. And so. I'm wondering, in addition to that almost like increased threat because of the environments that you're in or because you're on your own for the first time, you're in a new city, you don't have as many adults around you, are you seeing different ways that college students are Navigate through these challenges and deal with it after the fact, compared to maybe adults, , or individuals that are no longer in college.
Dr. Judith Joseph: I think that even in college, people joke about it. it's normalized, and I do think that even adults do that. You know, they normalize it. They're like, oh, you know, they're just being kids, or that's just the party culture, or like, It's almost like a, well, you got to look out for yourself, not like, wait, this shouldn't be happening, right?
Yeah. , like it's, the onus is put on the potential victim, and it just is not right. So I do think talking about things openly, powerful. there's a lot of shame around these conversations. People feel uncomfortable talking about it. And I think a lot of that is because It's almost like you feel like if you talk about it, it'll happen, which is so not true.
The more you talk about these things, the less likely they're going to happen. And also some people have like childhood trauma and it just brings up, emotions that they don't want to deal with, which is understandable, but, you know, acknowledging that that avoidance is a result of trauma. , and I also think that there are like sticky legal implications because, , some university policies are not the best, right?
They don't necessarily protect. people who are more likely to be victims. , so I do think that it's, you know, it becomes a very complicated issue. But what I've seen in my clinical practice is students who get involved in organizations. Like when I was, , an undergrad, I got involved in the Rape Crisis Center because I wanted to do something about it.
Right. I was hearing stories, , across the country about, these, , , issues specifically targeting women. And I was like, well, I want to be a part of the, of the solution. So, you know, getting involved is really empowering because when you hear the statistics, it can be depressing. It's daunting, but it doesn't have to make you.
Sadie: I would also love to ask you, obviously you work a lot with college students and you, I'm sure as you continue to treat these populations, you end up working with a lot of individuals who are either post grad or further along in their journey of life. If you had certain skills or recommendations or resources, or even just like this is when it's time to look for a psychiatrist or a therapist that you wish college students and young adults were aware of that would prevent so much of these challenges, , and mental health issues like we talked about at the beginning of this episode.
What would those recommendations and pieces of advice be?
Dr. Judith Joseph: Because in high functioning depression in particular, I see a lot of, well, I'm not as bad as other people. People have it worse than me. No, like that's not, that shouldn't be the, the barometer for getting help. Right. If you're having feelings and you're having those thoughts, like I'm not deserving of this, or I don't have as bad get help.
Right. Because I think that, things like high function, depression are pro drama. They're like leading up to something that's. That could be really, really devastating. Right. And so it's easier, especially from a research point of view and a clinician point of view, it's easier to support someone before it's gotten to a point where it's very, very difficult to support them.
It's way easier in the early stages and they have better outcomes. So like, if you, if you're someone who's like, I'm not as bad as other people start thinking about getting help because yeah, you may not be as bad as the people, but do you want to get there at that point? It's really difficult. , I always, , you know, joke.
And I say you don't want to start looking for a therapist when you need one, because you know how it is that waitlist sucks, , and your options are going to be limited. So it's better to have someone when you don't feel like you need them. Then to wait until you do,
Sadie: especially to build that relationship, to be able to talk to them and trust them and have them like know when you're hiding things and like when you're not doing as well.
If you have that in place when things get bad, it's a game changer.
Dr. Judith Joseph: Yeah, like I always, I always say to my clients, like, you know, like when you're late and you're looking for your keys and you're just like, where are my keys? Where are my keys? And they're like right in your hand or they're right in your purse.
It's the same when you're in crisis and you're like, I need a therapist. That's like the worst time to find someone, right? And that's why a lot of people have really bad experiences with therapy because they're like, well, I just had to find someone. So I picked the first person that was available. Well, that's like the worst way to pick something, right?
Like, we, I mean, I love my nails and my hairs and stuff like that. Like. I'm not going to look for someone when my nails are grown out. I'm going to look for someone when I'm, you know, I want, I want to be relaxed, enjoy the experience. Why don't we take our therapist like that? We wait until we're in crisis mode.
Sadie: I was doing my nails right before this. I'm like half done. We have our little nail drill going on. So I 100 percent feel you. It's so funny. I even think like if you're in crisis, you go to a therapist you've never met with before and they're like, okay, so here's your 30 page intake document today is just to get to know you.
And the person's like, oh my God, I need help. But they're like, that's not on the agenda for today. We haven't gotten there yet. So I think that's really, really great advice to have that resource set up, even if it's like biweekly, every three weeks, those are totally options that you can put in place and set up.
Dr. Judith Joseph: Yeah. I mean, like when you're, when the human brain is stressed, it makes the worst decisions, right? The absolute worst decisions. So do you really want to make the worst decision with the person who is you entrust with your most delicate organ? I don't think so. You want to, you know, if you know that you're someone who has anxiety and you get stressed, make that appointment months ahead of time.
You may not need it. You may be fine by the time the appointment rolls around, but then that's great. The worst thing is when you need a therapist and you're in crisis because you may find someone that's not the right fit and then that's not a good experience for either person. A
Sadie: hundred percent. Well, Dr.
Joseph, this was absolutely incredible. I'm so glad we got to do this. I know this is going to be so helpful to so many people. If everyone wants to listen to your podcast, Read about your research, follow you on social media. Where can they find you? You
Dr. Judith Joseph: can find me at drjudithjoseph at TikTok and Instagram.
And I just started a newsletter because I get DMs all the time. Like, are you taking new patients? Can you be my therapist? Well, in my weekly newsletter, I put in my tips and I have, I drop a new podcast every week. So, , it's in a way you're getting some therapy tips, , but definitely use them alongside your current treatment.
Sadie: Yes, I love it. Well, thank you so much.
Thank you so much for listening to this week's episode of she persisted. If you enjoyed, make sure to share with a friend or family member, it really helps out the podcast. And if you haven't already leave a review on apple podcasts or Spotify, you can also make sure to follow along at actually persisted podcast on both Instagram and Tik TOK, and check out all the bonus resources, content and information on my website.
She persisted podcast.com. Thanks for supporting. Keep persisting and I'll see you next week.
© 2020 She Persisted LLC. This podcast is copyrighted subject matter owned by She Persisted LLC and She Persisted LLC reserves all rights in and to the podcast. Any use without She Persisted LLC’s express prior written consent is prohibited.