88. The Neuroscience of PTSD, Traumatic Experiences, and Emotion Regulation feat. Madeline Bailey
listen to this episode:
Tune in and subscribe on your favorite platform: Apple Podcasts | Spotify | Stitcher | Google Play | Radio Public | PocketCasts | Overcast | Breaker | Anchor
Today's guest is Madeline Bailey—she holds an M.S in Neuroscience from Tulane University and has a B.S. in Psychology from the University of North Carolina at Chapel Hill. Her research interests are in neurobiological and molecular, specifically epigenetic changes, caused by stress and trauma, and how these later affect the development of mental health conditions. Madeline and I met through the Almost30 Podcast Accelerator—highly recommend to any podcasters out there—and connected over our shared passion for mental health! In the second half of this podcast swap (listen to me on Finding Your Freedom HERE) we discuss Madeline's mental health journey, navigating traumatic experiences/PTSD, ways we respond to traumas (bit and little t), what happens to the brain when we experience trauma and when this becomes PTSD, regulating emotions with/without PTSD, treatment options, epigenetics, and more!
Madeline's Instagram: https://www.instagram.com/madelinebbailey/
Finding Your Freedom: https://pod.link/1496653089
This week’s DBT skill is the Check the Facts skill! Learn more HERE!
Mentioned In The Episode…
+ PodcastPro from Almost30 (tons of freebies and their YouTube is AMAZING)
+ EMDR
SHOP GUEST RECOMMENDATIONS: https://amzn.to/3A69GOC
Episode Sponsors
🛋This week's episode is sponsored by Teen Counseling. Teen Counseling is an online therapy program with over 14,000 licensed therapists in their network offering support with depression, anxiety, relationships, trauma, and more via text, talk, and video counseling. Head to teencounseling.com/shepersisted to find a therapist today!
☕️This week's episode is brought to you by Nutpods. Shop their delicious Vegan, Gluten-Free, Non-GMO, Kosher, and Whole 30 creamers today and use code 'SHEPERSISTEDPODCAST' at checkout for 15% off your order.
🍓This week's episode is brought to you by Sakara. Sakara is a nutrition company that focuses on overall wellness, starting with what you eat. Use code XOSADIE at checkout for 20% off your first order!
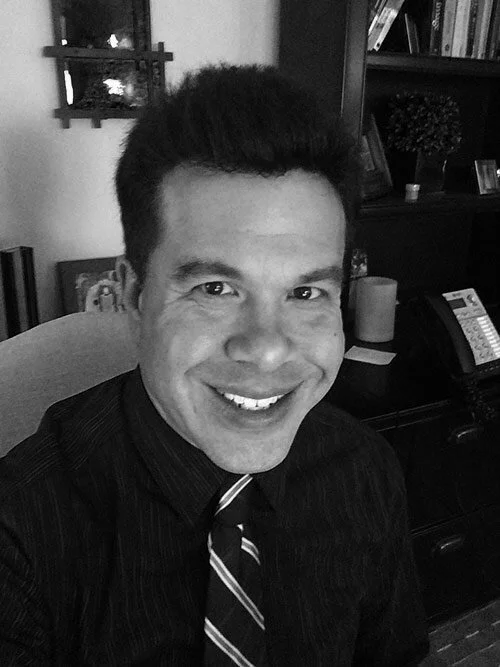
About She Persisted (formerly Nevertheless, She Persisted)
After a year and a half of intensive treatment for severe depression and anxiety, 18-year-old Sadie recounts her journey by interviewing family members, professionals, and fellow teens to offer self-improvement tips, DBT education, and personal experiences. She Persisted is the reminder that someone else has been there too and your inspiration to live your life worth living.
a note: this is an automated transcription so please ignore any accidental misspellings!
Sadie:
Welcome to she persisted. I'm your host Sadie Sutton. Every Friday, I post interviews about mental health dialectical behavioral therapy and teenage life. These episodes break down my mental health journey. Teach skills to help you cope with life and showcase testimonials from individuals, including teens.
Whether you've struggled yourself or just want to improve your mental fitness. This podcast is your inspiration to live a life you love and keep resisting this week on cheap, persistent,
Madeline: even have the awareness that there were traumatic things and that, you know, that trauma changed your brain and it changed your body.
I just felt like my body and brain were against me.
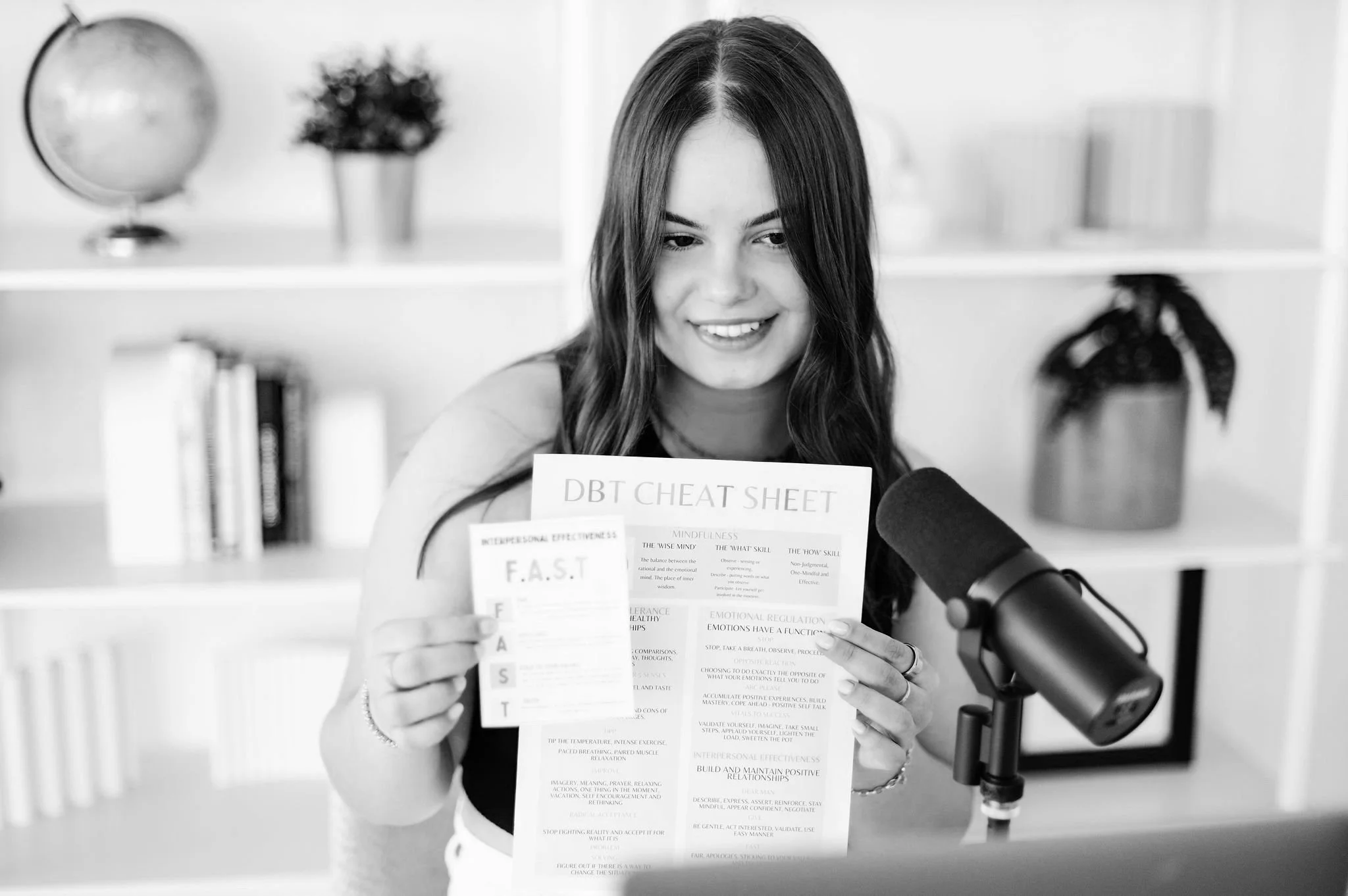
Sadie: This week's DBT scale is the check. The facts. Many emotions and actions are set off by our thoughts and interpretations for events, but not by the event themselves.
Think about it or Benz leads to thoughts, leads to emotions. Our emotions can also have a really big effect on our thoughts about the events that have occurred. So when we examine our thoughts and check the facts, it can help us change our emotions and therefore our actions. Here's what you're going to do. First. You're going to ask yourself, what is the emotion I want to change?
If you listen to episode 85, all about emotion, education, you know that the core emotions in DBT are anger, disgust, envy, fear, happiness, jealousy, love, sadness, shame and guilt, almost all of what you're feeling can likely be categorized into one or two of those emotions. So identify which one it is and ask yourself, what is the event prompting that emotion you're going to describe the facts that you observed through your senses. So what did you see? What did you hear the goal of this is to look at the situation completely objectively. You're also going to challenge any judgments, absolutes, or black and white thinkings that around.
The third step is to ask yourself, what are your interpretations, thoughts, and assumptions about the situation. You're going to think about other possible interpretations. You're going to practice looking at all sides of the situation and multiple points of view. And you're going to test your interpretations and assumptions to see if they truly fit the facts of the situation for if you're going to ask yourself, are you assuming a threat?
If so, you're going to label that threat. . Assess the profitability that that threat will actually occur and think about as many other possible outcomes as you can fit. You're going to ask yourself what's the catastrophe.
That's like the worst case scenario. So imagine that actually occurring. Imagine coping well with that catastrophe. So maybe you're problem solving. Maybe you're coping ahead. Maybe you're accepting that you're navigating that. And lastly, you are going to ask, does my emotion and or its intensity fit the facts.
If you are wondering what some typical responses to emotions are and what leads to like an over experience of an emotion, I highly recommend you listen to the emotion education episode, because I go into so much depth on that for every single emotion.
So you're going to check the facts that fit each emotion. And you're going to ask your wise mind, you're going to take into account logic and emotion and ask yourself, does this really objectively fit the facts?
So that is the check, the fact skill, one of my all time favorites and applicable to so many high intensity situations.
Hello. Hello and welcome back to Sheba assisted. I am so excited. You're here today. We have an amazing interview with Madeline Bailey. She is the host of the finding your freedom podcast. And we actually met through the almost 30 podcast accelerator. So side note podcasters, if you were ever looking to learn more about the podcast industry growing in monetizing a podcast or launching a podcast and just knowing the ins and outs of what goes into it. The podcast pro course from almost 30 is one of my favorite investments that I made into the podcast. Um, they open it up for. Couple of times a year, maybe it's once a year and before they do like a one week trial, so you can test it out and see what it's like.
And it was just the most amazing experience. It's an eight week course, and I will of course share on the podcast and on Instagram when they open it up again, but they also have a ton of resources and free downloadables on their website and their YouTube channel as well for the podcast pro has a ton of like free tips and tricks.
So I'll be sure to link that in the show notes and amazing resource. And I'm so glad I found anyways, Madeline and I connected through with that chorus. We both had a huge love for mental health and we'd both been through different mental health experiences. And so we had to do a podcast swap. And so I went on her show.
And talk to all about my journey with DBT and therapy and treatment, and it was just such a fun episode to do. And then she came on, she persisted for today's episode, and we talk all about the neuroscience of PTSD, traumatic experiences, emotion, regulation, and so much. So, this is an amazing, amazing episode.
I know you guys are all going to love it. If you do make sure to leave a review share on social media, you know, the drought, if you share it Instagram, I will make sure to repost you and give you a little shout out. My Instagram is at sheep resisted podcast, and I love seeing you guys listening and makes me so happy.
As I wanted to mention, I think I would have said this in last week's episode also, but if you want to watch the podcast episodes, they are on the sheep assisted YouTube channel. So I'll put a link in the show notes, but I am on my game. So if you want to see the conversation happen, not real time, but you know what I mean?
That resource is available.
I also am starting to think about what I want to do for the next couple of months of content. And we are coming up slowly but surely on mental health awareness month. And I just want to make sure that the episodes and content that I'm putting out is what is helpful to you guys. So I've been seeing on the analytics side that you guys are loving the solo episodes.
I'm going to keep doing those and make sure that they're really well thought out and researched and just full of value because I really enjoy those. And it's, it's really fun to share what I learned from my journey. But if there's anything else you want to see, whether it's like more real, it's more tick talks, more day in the lives, more episodes on a certain topic.
Be sure to let me know, and I will do my best to make that happen. So with that today's guest is Madeline Bailey. Like I said, she holds an Ms in neuroscience from two lane and has a BS in psychology from chapel hill, go tar heels. My parents went to chapel hill, so we are big fans over here. She has a ton of research experience and neuro-biological and molecular epigenetic changes that are caused by stress and trauma. So Madeline has so much insight on not only her own experience and the insight that she gained from that, but the research and neuroscience side of things. So this just creates an amazing well-rounded episode jam packed with value, and I know you'll love it.
So with that being said, let's dive in.
Thank you so much for joining me today, Madeline. I'm so excited to have you on the show and to dive into your story, to talk about trauma and PTSD from a neuroscience perspective, I just can't.
Madeline: Yeah, me too. I'm super excited.
Sadie: This is actually like the second half of a little podcast swap.
So listeners, if you haven't already listened to the part on madeleines show, it's called finding your freedom. It'll be linked in today's show notes, but we talk all about DBT and treatment and my story. And so that was a really fun episode to do, so I can't wait to round everything out in this swap and hear your side of your story. So let's start with going into your journey before we dive into the scientific perspective and add more context, add more information for listeners let's hear about you.
So take me back to the beginning of your journey and, and your mental
Madeline: health. Definitely. I think it's always hard to pinpoint a beginning because I think once you start this healing work, you can, you know, go back to two years old and see a beginning of like a mental health challenge or something like that.
But I think the really like the beginning of my story was my junior year of college. Up until that point I'd been. Pretty kind of normal functioning kid with, you know, some other issues that I figured out later. But during that time, my mom was going through her own mental health kind of crisis.
And, you know, my mom had always had depression, but it wasn't something that we talked about. It was always kind of whispered in corners and we didn't want. Address it. But my mom was let go from her job and that kind of triggered like a depressive episode. And yeah, I think there was just like a lot of complex messaging for me.
And it just got to a point where I felt like it was my job to save my mom, which was just a crazy amount of stress to put on someone that's only, you know, like 20 years old trying to navigate. You know, a hard semester pre-med and then also feeling like I was responsible for, you know, keeping my mom alive and you know, so much compassion for my mom.
She didn't want me to feel like that. And you know, I think when you're a kid, you just internalize certain things from your family and they have really profound impacts on you. And I was actually like a psychology major, but no one in my family really talked about therapy or getting. So I could just tell that I was under this overwhelming amount of stress.
I wasn't eating. I had like a hard time focusing, but I didn't really have the resources to do anything at that time. So I kept just kind of moving along with my life and doing the best that I could. And, you know, after that experience, I really struggled to feel like the same battle line. Felt different.
I felt like I was struggling with depression after that. I felt like a lot of intense shame and guilt. Like I could have done something differently or I could've done something better. And I just really, really struggled after that and kind of tried to just not address it at all. And right after that happened, I actually studied abroad in Australia.
So I was on the other side of the world from my family, concerned about my mom and you know, so many different things were happening. And then. You know, fast forward to senior year of college, and I'd kind of tried to avoid dealing with any of that. And then, you know, the stresses of what am I going to do with my life.
Everybody's getting jobs going to like a very intense undergrad experience at UNC. The pressure of that just started to wear away at me again. And I kind of got in the same head space. You know, it was kind of doing the same behaviors that I was when I initially went through that trauma where I couldn't eat, I was really stressed all the time.
I lost like 20 pounds. I just was anxious constantly. Like there would just, wasn't a second that I wasn't anxious. So kind of after that experience really, after I graduated college was the start of me actually looking at these things. Kind of starting to explore ideas outside the typical kind of mindset of psychology.
Like I'd been to a therapist a little bit, and there'd been like a decent amount of talk kind of about medication, which, you know, no shame for medication, but I just felt like that wasn't right. For me, I felt like I just like knew it in my heart that this anxiety that I was feeling, wasn't just about the transitional.
From college. Like I knew that there was something deeper and I didn't, you know, I talk about it now. Like I knew the connection to the thing that had happened with my mom, but it was all subconscious. So, you know, I kind of started this journey of slowly looking at things and a really big turning point moment for me was actually my dad saying to me, you know, you're not the same Adeline anymore.
Like you default to sadness. Now you don't trust yourself. And you're just super anxious all the time. Like, I've just this, wasn't how you used to be. And like, I don't know how to change it or what to do, but like, you're just not the same anymore. And that was a really jarring thing to hear from my dad and kind of realized like, wow, I need to take care of this and kind of start my healing journey.
So that looked like, you know, getting into therapy. Exploring kind of spirituality exploring. Different healing modalities, because another part of that experience as well was I had gone to undergrad to be a doctor. And then I kind of started questioning Western medicine. So I was having this kind of like identity crisis of building myself around this idea of being a doctor.
So when I started my healing journey, it was to kind of address the trauma that had happened. And then also all of these realizations of. Perfectionism and how to keep myself safe my whole life. I had put all these standards that I needed to have and to pass, to be worthy of love. So, you know, being a doctor, you know, being this certain weight, looking this certain way, like I clung to perfectionism till like a point where I was like, this is not serving me anymore.
So that was kind of the start of my kind of healing experience. Yeah. Deeper within myself, but there've been so many bumps along the way. I mean, when my therapist told me linear, it is not when my therapist first told me that she thought I had PTSD. I literally got in my car and drove to California east coast.
Oh my God. And then I came back and I was like, okay, I'm ready to address
Sadie: this. Let's try that again. Oh my
Madeline: goodness. So yeah, it's been a really interesting journey. And through that drive actually to the west coast, I was in a really big period of feeling lost and not knowing like what my life was gonna look like.
Without being a doctor as well. And in that, you know, 45 hour drive to the west coast and not
Sadie: so long, for some reason I didn't even process that. It was wow.
Madeline: Yes. It, it clicked to me that neuroscience was exactly where I was meant to be and made so much sense with all the things I had been interested in.
So kind of from like there, and that experience, I started actually like looking. You know, the traumas in my life, I started looking at kind of like the brain and meditation and all these other aspects, but it was definitely not linear and a slope like progression. I have so much self compassion for people being scared to start, because I felt like I was opening like a tidal wave of experiences that I had numbed out because.
My perfectionism as well. The ideal that I was going for was emotions. Aren't perfect. So I can't feel those. And I just have to be achievement oriented and, you know, stuff, all those feelings down. So when I first started going to therapy, it felt like the flood gates of all of these emotions that I had.
That's so interesting.
Sadie: I remember the exact same thing. It was a little bit different though, but I also connected that like emotions aren't perfect. And for me, it was related to my relationship with my parents. And I really believe that I would never be good enough for them. And emotions would make me less good enough for them because they were less.
So I would not express emotions around them, which made things super difficult. And that was like a very intensive process to like get to the point where I could be like, I'm not okay. I need help because that was something that like I had to voice to them because I was obviously still a teenager. And I, I still experienced the same thing with like the flood gates where.
When I, I only really noticed it in therapy, I would say, or if I'm in a really emotional situation, when I'm talking about something, it's like, Logically connect that I need to cry, but my like eyes just like start crying and I like can't help it. Like, if I'm like upset about something or I'm in an argument, like that feels connected.
Whereas like in therapy, sometimes I'll just be talking and I'm like, I'm just going to start crying. Now you can ignore that. I'm just still going to keep talking about what I'm going to, but it's like, those suppressed emotions are still coming forward. Even if they don't see like the necessarily fit the facts of like what I'm talking about in that moment.
Th there are still there.
Madeline: Yeah.
Sadie: This week's episode is sponsored by teen counseling. You guys have heard me talk about them so many times before, because I am such a huge proponent of therapy and mental health support when you need it. So teen counseling is the teen branch of better health, and it's an online therapy program with over 14,000 licensed therapists in their network.
And they offer support on things like depression, anxiety, relationships, trauma, and so much more. Teen counseling offers, talk, text and video counseling all with licensed therapists. What you're going to do is you're going to go to teen counseling.com/jeepers history. You're going to fill out a super quick survey about what you were hoping to work on on therapy. So whether that's stress related to school or relationship with your parents or feeling depressed, whatever it is, you're going to talk about that in the survey, they're going to ask a bunch of questions and they're going to match you with a therapist that means to you.
From there an email sent to your parents. It's super vague. I tested it and sent it to myself and it Sadie or whatever your name is, is hoping to work with a licensed therapist from teens counseling. Please click below to learn more and give consent for treatment. None of your information about what you're hoping to work on is disclosed.
Your confidentiality is completely protected. And from there you are able to start working with a therapist. So, if you are looking to dip your toe in the water and begin your therapy journey or continue it, if you are like me and have been around the block a few times, you can head to teen counseling.com/
Again, that is teen counseling.com/cheaper assisted to find a therapist.
Madeline: I think for me, I just like, I guess, I guess I would call it kind of like a spiritual awakening or kind of just like a really quick increase in awareness where I just started to realize all these things about myself. And it also felt like I was like looking at the world around me and it felt like I was seeing trauma everywhere.
Yeah. I think I was like starting to get to a point with the mental health world where, and I know this wasn't, you know, exactly your story, but I was seeing like, wow, trauma seems to be the root of so many of these, these things, like, you know, I took abnormal psychology in Colorado, great class, love them.
I was, you know, looking at all those things. And I was like, I feel like trauma is like the root of so many of these things. This like kind of increase in awareness. You know, I would be around my parents and I would be like, they're doing this behavior because of this thing that happened in their childhood.
And like, I wouldn't say it, but I could just like, see the reasons for people and how they were acting from, you know, their subconscious. And it was like a very like jarring experience to be able to see so many people acting from like these pain points and, you know, see myself acting from these pain points in that I'd never been away.
That I was doing that before, until, you know, I was 22.
Sadie: Yeah, no, I, I relate to that a lot because as I continued along my treatment journey at the beginning, I was firmly like, there's no reason why I'm depressed. I'm just depressed. And I was, there was like no major loss. Like there was no none of those big T traumas that it could explain the magnitude of depression and anxiety that I was feeling, but the further and further.
That I get away from like that initial rock bottom and the more emotional distance there is, the more I can reflect, the more I can see like the little T traumas and I can be like, okay, well being invalidated in a home environment, even if it wasn't completely falling apart, it still could lead to me feeling like I didn't deserve love and that I wasn't good enough, which could lead to these feelings of depression.
And so acknowledging that I had experienced. Little T traumas. And that was okay. And because I totally had the belief in my head where I was like, I shouldn't beat oppressed. Like, there's nothing that's gone wrong. Like I have loving parents, I have a family that's intact. I have so many resources at my fingertips, like what is happening?
So it was kind of making that connection and being like, okay, maybe think everything. Wasn't perfect. And that's okay.
Madeline: Yeah, I think that's so important. And that was like a really big part of my experience was like validating the small traumas. And I, I think like a really important thing to highlight too, is that, you know, people who have gone through traumatic experiences, you know, big or small experience, a lot of shame and a lot of people dissociate as well.
So a lot of people forget, quote, forget things, or they invalidate the intensity of. You know, when I first started like looking at these things to my therapist, I would never have been like the thing that happened with my mom and her mental health. Like I never was like, I was like, that's not a trauma.
That's just like a hard thing. And you know, now I'm able to like validate that that was, and some things that happened to me in high school that I never processed that came to light and were part of the like flood gate feelings, like, oh, that is a trauma. But I was, I myself was so invalidating that those things were.
Traumatic because emotions just weren't really discussed. So I thought I don't, I don't know. I thought you just got through things. Like, I didn't even have the awareness that there were traumatic things and that, you know, the trauma changed your brain and it changed your body. I just felt like my body and brain were against me.
Why can't I just be happy and normal, you know,
Sadie: I think that's a really universal experience with people that are struggling and it's, it's a hard thing to work through. So you have, we touched on this a little bit, but you have a really interesting perspective on things like trauma and PTSD because of your background in neuroscience.
So I want to. Add that to the picture and give listeners more insight, because I think it's really helpful to apply to their experiences with big T little T traumas and just kind of understanding, like you're saying how that impacts how individuals function and relationships. So I want to start with what happens to the brain when someone experiences trauma, and then kind of going from there, how the brain and the body change when you develop PTSD.
Cause there's kind of that distinction. And we've been talking about this a lot in abnormal psychology. A lot of people experienced traumas, but not everyone develops PTSD. And so there's kind of like all the questions of like, okay, what makes us two people different? And that's a can of worms for another time, but kind of talking about what happens when someone experiences trauma.
Madeline: Yeah. And I just want to say, like, I'm so passionate about talking about the science behind, like what happens to your brain after you experienced trauma or what happens to your brain when you're depressed? Because that information gave me so much self-compassion. That it's not just like in my head, like it's a biological process that's going on.
That is a little bit like out of my control and like it's okay to be feeling how I'm feeling, but just to give a little bit of context. Yeah. Like I think that's so important. And just to give a little bit of context, like I was, you know, I was pre-med and undergrad and I was a psychology major, so I had a decent amount of neuroscience knowledge.
And then I got a neuroscience master's degree and mainly kind of focused on. You know, trauma and mental health and neuroscience and those factors of what you know is going on in the brain. And I think your first question is like, what happens when you experience a trauma? Like in that moment, right? Yeah.
Yeah. So when you experience, you know, stress or an actual trauma in that moment, there are two processes that are going on. So it's, you know, your autonomic nervous system and then your HPA access. So the autonomic nervous system is that parasympathetic and sympathetic. So everyone knows like the typical example of like, I dunno like a bear or something scares you, but you know, that could be, I don't know, that could be like someone following you down an alley that could be like an actual, like sexual assault that could be, you know, in terms of a stress that could be like you ruminating and thinking about a test.
You know, all of those have like the ability to trigger this autonomic response and this hormonal response. So just to kind of break it down a little bit more in the brain, just to like focus on a few brain areas. So the medial prefrontal cortex is kind of that area of the brain that can kind of illogically process.
Say like you're experiencing like a stressor. The prefrontal cortex can kind of like, like lessen the intensity of like the amygdala and the fear that you're feeling. So there's the prefrontal cortex, the amygdala, the hippocampus, and the hypothalamus that I'm going to talk about. So the amygdala is that place in our brain, that's kind of processing that fear and the prefrontal cortex can kind of like tone that fear response down to an.
The hippocampus is memories. So when we're feeling that kind of fear and the amygdala that has connections to the hypothalamus, which the hypothalamus is kind of the hormonal response center. So the amygdala kind of triggers that neural response, which is the sympathetic autonomic nervous system. And then also triggers a hormonal response.
So the neuro-transmitter response is going to be. A faster response and it's going to be epinephrine and norepinephrine in the body. And that's kind of like mobilizing your body for, for an attack. You know, it sends like blood to your muscles, takes it away from digestion, kind of mobilizes resources in an evolutionary fashion.
When we used to be like cave people, you know, fighting off an actual attack. And then as far as the hormonal response, that's going be. You know, the hypothalamus interacting with the adrenal glands, and that's going to be sending that cortisol throughout your body, which is also, I think we think about cortisol kind of the stress hormone is a bad thing, but in the short term, it's, you know, hugging you alive.
Yeah. It's what keeps you alive when something really stressful is going on. So that response is not a problem at all. And that's like our body helping. What is a problem is either in chronic stress where that stress goes on too long, or when the stressor is too intense and the functioning of our body can't like tamp down on the response.
So our cortisol signaling gets all off and also like our neuro-transmitters signaling gets all off. So when you have like a really intense trauma and people with PTSD, Those connections from the medial prefrontal cortex that would usually kind of calm down the amygdala when it has fear. They're not really as active, they're less connected than people who don't have PTSD.
So you see anything that relates to that a traumatic event. Amygdala acts up, you have all those hormones and all those neurotransmitters in your body, and you're really active. And you know, one of the symptoms of PTSD is, you know, hypervigilance, those people are kind of on edge all the time. Like they can't really sleep.
They feel like constantly this like anxiety feeling, which is related to that.
Sadie: This week's episode is brought to you by Nutpods. I am a huge iced coffee fan, but obviously I'm at college and living in a dorm. And so my resources are limited and iced coffee is not the most college friendly drink all the time. They have it down to a science. I have the most amazing eyes trades from Amazon.
I'm a huge fan of the Starbucks cold brew concentrate, which you can also get on Amazon. And my third key is not pods.
Nutpods creamers are beacon gluten-free, non-GMO kosher and whole 30, and best of all, they taste amazing. They have so many amazing flavors, both an unsweetened and sweetened varieties. My favorite is French vanilla and sweet cream. They're just delicious and tastes just like the Starbucks vanilla sweet cream cold brew, which was one of my favorite drinks to get when I'm at Starbucks.
And the best part for me is because they are vegan until you open them. You don't have to keep them refrigerated. So this means I can stock up, not have to worry about the fridge space and enjoy my creamer as I want to.
So if you want to check out nut pod, you can go to nutpods.com and use code cheaper assisted podcast at checkout for 15% off your order. So again, that is code she persisted podcast at checkout for 15% off your order. And the link is in today's show notes.
So are there any other significant changes that happen when you go from just experiencing a trauma to having PTSD?
Madeline: Yeah, something else that I kind of wanted to say about that in teams and something that I think is really interesting is that there are studies that kind of look at the age that you experience a traumatic event because the earlier that you experienced a traumatic event, it's going to have different effects because different brain areas are still developing.
So say you experience a sexual assault in high school. The prefrontal cortex is still developing. And, you know, it could like literally cause damage to that as it's developing, which would be more intense than versus when you're already like 25 and it's fully developed and, you know, say you were physically abused in elementary school, deeper brain areas are developing.
So it affects the proper developing of those. So I think that's like a really important point too, that timing does matter on like what areas are affected as.
Sadie: Wow. That's so interesting. I've never heard that before. That's that's crazy to think about we talked a little bit about emotion regulation and how the prefrontal cortex can ask the amygdala and the hippocampus.
Are there any differences between someone who. I mean, we did kind of touch on this, but differences between someone who has PTSD, trying to regulate emotions versus someone that is just normally trying to regulate emotions and what makes that difficult from like a neuroscience perspective.
Madeline: Yeah. I mean, I think if you've never tried to regulate your emotions, of course, that's going to be a challenging experience, but someone with PTSD, it's going to be a lot more challenging.
Because the amygdala is going to be a lot more active and there's going to be less connections kind of already there between the amygdala and the prefrontal cortex and something I wanted to say with that too, kind of related to your last question is that there's been a lot of research also on like inflammation and cortisol.
And the immune system also are like reacting in this process. Cortisol when it's active for too long creates like an immune response and increases inflammation as well. But as far as like trying to emotionally regulate with PTSD, another thing that I think is really important and someone I really look up into the field of this is, you know, the body keeps the score by Dr.
Bessel van der Kolk. I think trauma's like really a bodily experience and the way we start to. Tamp down the amygdala is that it needs to complete the cycle that it was trying to complete. So that's why I'm a huge proponent of, you know, getting into your body and more like somatic therapies and like, especially like EMDR, because, you know, just talking about the trauma again, isn't really enough in a lot of cases to make that tamped down.
That's also why like you know, like extinct. And doing like therapies that make you go through, I'm blanking on the name of that therapy. Do you know what I'm trying to say? Exposure, exposure therapy is really important because you need to, I'm not sure if like your audience kind of knows like what classical conditioning is, but basically
Sadie: ugly skin or the box with the rats.
Everyone.
Madeline: Yeah. Basically with PTSD. Things that are at all related to the traumatic event, start to be prepared and they trigger the same response that you would have from the initial trauma. So that's why it's also really important to have exposure therapy, because you need to like detach those, those kind of associations.
So you can kind of like complete the cycle in your body, but also, you know, not be triggered by. A red pen, because there was a red pen on the desk of this person that like hit you or something, you know? So I think that's a really important part of the process as well. Yeah.
Sadie: So you mentioned EMDR like a super quick explanation of what that is, would be helpful for listeners and then from a neuroscience perspective, like what happens when you do EMDR treatment?
Madeline: Yeah. So EMDR has. Eye movement, desensitization therapy. And as far as what happens in the brain during EMDR, people are still confused on what happens. The guy that founded EMDR. I think the story is that he was like on a walk in the woods or something and was like moving his eye and some certain way in the woods and realized that he felt more calm about his trauma.
So like a really random story of discovering this and basically kind of the process and therapy is you recalling kind of a traumatic event and the core beliefs that, that traumatic event made you feel. And then like moving your eyes and like different motions and some kind of theories on how that works is, you know, it's kind of like getting you into a calm state, I would say, and engaging your body at the same time as you're recalling the trauma.
And I think another thing that is also helpful with. Looks into the core beliefs that, that trauma made you hold. And I know in, on our episode, we did, we talked a lot about core beliefs and how that can be a big changing factor with that. But as far as the exact mechanism, they don't really know.
Something I think is really interesting is there was a study done showing that EMDR was able to kind of change the epigenome. So just for anyone that's listening that doesn't know what epigenetics are. You know, we all have genes. That's our genome epigenetics is basically how life experience can turn off and on genes and something I've been really interested in is how do these genes kind of change due to trauma and due to different psychiatric illnesses?
You know what therapy is potentially like reverse these changes. And I think that can be really interesting to look at and see what's actually happening at like the gene expression level. You know, different psychiatric conditions. Yeah. The
Sadie: eye movement. I was listening to an episode of the Hebrew in lab podcast, which is my new one of my new favorites.
And it was with Dr. Matthew Walker, who is a dream podcast guest I've pitched him. He hasn't responded yet. We'll see folks. But they were talking about how REM sleep as the stage of sleep when you're like emotionally processing. It's like that scene in inside out when all the emotions get cataloged and put in your long-term memory.
And so they're no longer like at the forefront of your mind. And so this is me completely speculating, but it makes me think of that because when you're in REM sleep, your eyes are moving back and forth really quickly, which is super. To that stage of sleep. It doesn't happen during the rest of the night.
And it's also the only other time of the night when you're cataloging processing through those emotions. So it's really interesting that that also is what's going on in EMDR. And I'm not sure if it's the same movement or if there's any connection there, but that's super interesting.
Madeline: Yeah. Yeah. I've made that connection to, because actually I went to a lecture on sleep and they were talking about how so in PTSD sleep is a big problem.
Like a lot of times. You know, aren't going into, like, if they're going into REM sleep, they're having these really horrible nightmares. So, or they're just really not sleeping well, because they're so like hypervigilant all the time. And in this talk, they were basically talking about the fact that people can't get these, these can't get into REM sleep and can't get good sleep actually impacts.
Then being able to emotionally process the trauma, you know, like if they could get better sleep, they could consolidate some of those memories and kind of process the emotions of the trauma. Because sleep, I, I know like pretty much everyone listening probably knows the experience of you're really anxious or like feeling bummed about some conversation or a test or something.
And then you go to sleep and you wake up the next morning and you're like, yeah. You're like, that's all that big of a deal. So yeah, sleep is like really important and interesting. And yeah, I love the humor men lab podcast. Like Andrew humor man is definitely a dream guests. And I sent him an article one time and he responded on Instagram.
I love it.
Sadie: No, he just has so much insight. It's crazy. I definitely have to like space out when I listened to that, because if I were to listen to that every day on top of going to classes, it'd be like too much information, not retaining anything.
Madeline: I have to take notes on his episodes with their stuff thorough, but I actually emailed him before.
Started the podcast. And before he was. Kind of Joe Rogan. Cause I think that's what blew him up, but not
a whole other conversation, but when he, he only had like 20 K followers on Instagram and I like DMD them about an article. And I was, I was trying to work in his lab. Actually. I sent him an email. Oh my gosh, he didn't respond. So I ended up at McLean instead. So we love
Sadie: McClain. We love special place in my heart.
This week's episode is brought to you by Sakara. Sakara is a nutrition company that focuses on overall wellness, starting with what you eat. They have an amazing meal plan service, where they deliver vegan. Gluten-free non-GMO you name it? Meals to your door and not everyone realizes this, but you can order just lunch, just dinner or even just breakfast if you want to. So maybe you're like lunch and dinner I'm sat, but I really struggled to get a good breakfast end. You can order Sacara just for breakfast. They will deliver your meal plan to your door at the week that you order for.
And they have the most amazing gourmet delicious recipes with the freshest ingredients. They're so creative and delicious. They also have a ton of wellness essentials. My two favorites you have to try, or the chlorophyll deep talks drops. I know you've seen them all over Tech-Talk but my favorite part is that you can add them to your water.
You get all the benefits of chlorophyll, but it doesn't add a taste. I thought it was going to taste like green and weird and linked greens powder. And it doesn't, it literally does not have a taste at all. My other favorite of theirs is their beauty chocolates. They have collagen and nootropics in them. So they are helping you get clearer, brighter, glowing skin while eating chocolate. And it doesn't get much better than that. So, if you want to check out Sacara, you can use code XO CD at checkout for 20% off your first order again, that is code XO sadia@checkoutfortwentypercentoffyourfirstorderatsakara.com or use the link in today's show notes.
So. With all this insight information on neuroscience and you haven't gone through these experiences, what stands out as things that you actually implement into, into your healing and your daily life? What are things where you're like, the evidence shows this. I tried and true love this,
Madeline: that kind of thing.
Yeah. I think I'm like a combination of like, I feel like my brand or who I am and my healing journey has been a combination of like science and stuff. So it's like implementing the things that I know that our research back that makes sense to me scientifically, but also like allowing the spiritual and the mystic to be healing as well for me.
And I think like a really big difference through going to this experience and going through therapy and learning about neuroscience is, and I had a guest on my podcast recently and was describing this. The climate of my mind is so different than what it used to be. Like. There are just so many thoughts of love and self compassion and, you know, thoughts that promote resiliency, thoughts that, you know, when something goes wrong, I'm just like kind to myself now.
And I also feel like I just have, I feel like surrender and acceptance has been like a really big part of my journey. So I think with neuroscience specifically, just knowing that whenever I feel a certain way, you know, whenever I feel anxious, I was feeling anxious yesterday that this is meant to help me.
This will pass this. Isn't, you know, this isn't that big of a deal, because I think before in my healing journey, I would get anxious and then I would be mad at myself for being anxious. And then I would be more anxious because I was mad at myself for being anxious. And then I just like, wouldn't you mean.
Leave the house. And I think now just, I think there's so many things, but like the biggest thing for me is self-compassion and as far as kind of like daily habits, it kind of, it looks like a lot of times where my phone is on airplane mode. It looks like a lot of meditation. It looks like we didn't touch on nutrition in this, but it looks like also being really mindful of.
The foods that I put into my body and drinking enough water, and I'm still in therapy now. And I, you know, see my therapist every two weeks. I'm always, you know, checking in with myself and I think another big difference now, too, is when I experience an emotion, I don't go to the old coping strategy of staying as busy as possible.
I pause with it. I get curious about it. I let the trigger exist in my body. I trace back to what is the story here? What is the truth here, you know, and I think that is a really big part of my pro I literally. I wish I could have like scanned my brain before everything happened. And now, cause it feels like a different brain that I have it's I
Sadie: should, because I remember it, my claim, this is so random.
They of course were ruling out any like physiological issues or like hormone issues for like why could be so crazy depressed. So we were like, is it a thyroid issue? Your thyroid has been acting. Which like, as my thyroid has never been a problem since I recovered from depression, that's a whole other interesting thing to unpack.
But at one point there was the question of like, did I have a brain tumor? Because there was some other symptom of like always being tired. There was something else I was experiencing in addition to the depression where they were like, eh, this could line up. We'll see. And so I got all of the. Brain scans done.
And there was one where they're like, we can't really tell let's do it with contrast and then I get another round done. And so I have those scans from that time and it'd be interesting to see how things have shifted and changed, but
Madeline: yeah, yeah, that is super interesting. And that makes me think, like I was listening to something, maybe a podcast with like Dr.
Amen, who I like really looked at him up to him as well. And he was talking about like, I think he was like his nephew or something. Basically showcasing like anti-social behavior, like was killing animals, was doing all these things that seemed like very out there and out of character and everyone in his family was really concerned and they like put them in a brain scan and he literally had a brain tumor.
They took out the brain tumor. He was fine. None of those behaviors were occurring anymore. Like I think we just don't think about the fact that something that blew my mind and my masters is. We say like, is there any thought process that isn't biological and like me thinking about what I'm about to say next is like a neuron communicating to another neuron and like a series of chemical reactions happening in my body.
As I'm having this conversation, that's just. Really mind blowing to think of that all happening to control everything that we're doing, or I know
Sadie: it's crazy. And I think it's very grounding and reassuring because again, we get so in our heads and we kind of our own worst enemy. So to have the science backing up that like when you're overwhelmed and you're having.
I thought processes. It's not necessarily like a reflection of you directly. It's your body doing its job. It's trying its best. And it's something that's kind of out of your control and that's definitely reassuring.
Madeline: Yeah. I think, I think something I wanted to say as well that I think like the thoughts that are in our mind are formed from the reality of who we are from like our families.
And a big part of my healing too, was like connecting to the authentic self and figuring out who I really was because I realized all the thoughts I was having was based on my conditioning of who I was meant to be based on how I was raised. So that's a whole other thing to unpack it, a whole other conversation, but no, that's so
Sadie: interesting.
So, so much insight here. I know listeners are going to find this really helpful, whether it was a little tear, a big T trauma they've experienced, or they're just curious about neuroscience, where can listeners find you to continue consuming your content and learning more about neuroscience and.
Madeline: Yeah. So I'm on Instagram Madeline B Bailey, and then my website is Matt online, be bailey.com.
Then my podcast is finding your freedom and that's on apple podcasts and Spotify. It's a lot of spirituality and like connecting to your authentic self, but I'm planning to do more neuroscience thing. Open to any suggestions and would love to talk about this more and plan to eventually do some like master classes and teach on these topics, because I think everyone can be empowered to know more about their brain.
Yeah.
Sadie: I love that so much. Well, thank you so much for coming on cheaper to stead. I'm so glad that we got to do this episode.
If you enjoyed this week's episode with Matt align, make sure that you listen to the first half of the podcast swap on madeleines podcast, finding your freedom. There's a link in the show notes to go and listen to that. And it was such a fun conversation, all about DBT and my treatment journey and therapy, and just so many amazing topics.
To recap this week's episode, Madeline and I discussed her mental health journey, navigating traumatic experiences and PTSD ways that we respond to traumas both big and little T traumas. What happens in the brain when we experience a trauma versus one, this actually becomes PTSD regulating emotions with, and without PTSD treatment options, epigenetics and.
If you enjoyed this week's episode, make sure to leave a review on apple podcasts and Spotify subscribe. So you don't miss next week's episode and follow along on Instagram at actually persisted podcast. Thank you for listening and I'll see you next week.
© 2020 She Persisted LLC. This podcast is copyrighted subject matter owned by She Persisted LLC and She Persisted LLC reserves all rights in and to the podcast. Any use without She Persisted LLC’s express prior written consent is prohibited.